Most diseases spinal cord(myelopathy) significantly affect the patient's quality of life and often lead to severe disability. Despite the variety of spinal cord diseases, their clinical picture has much in common. Symptoms such as movement and autonomic disorders, as well as sensory disorders and pain syndrome will almost always be present. The main types of diseases and pathologies of the spinal cord:
- Compression myelopathy.
- Non-compression myelopathy.
- Vascular diseases.
- Inflammatory pathologies (myelitis).
- Chronic forms of myelopathy.
- Degenerative and hereditary diseases.
- Malignant and benign neoplasms.
Let's consider the most common types and forms of spinal cord diseases.
Clinical experience has shown that nerve roots rarely remain intact when the spinal cord is damaged.
Compression myelopathy
Compression myelopathy is considered one of the most serious diseases of the central nervous system. With this pathology, damage to the spinal cord and nerve roots will be observed, leading to the appearance of characteristic symptoms of motor, sensory and autonomic disorders.
Causes
Taking into account how quickly the compression of the spinal cord and nerve roots develops, several types of the course of the pathological process are distinguished, each of which has its own cause. According to clinical practice, the following variants of compression myelopathy are distinguished:
- Sharp.
- Subacute.
- Chronic.
The acute form will be characterized by a sharp lesion of the spinal cord and its structures with a rapid increase in the neurological symptoms of the disease. Very little time passes from the moment of action of the damaging factor to the emergence of a detailed clinical picture. Most often, this condition can occur as a result of injury. spinal column or a spinal hemorrhage.
Of all the injuries of the spine, the most important in the development of acute spinal compression is a compression fracture, in which there is a displacement of the fragments of the vertebrae. A typical example is a diver's fracture. It is observed when hitting the head on the bottom while jumping into the water.
Many clinicians identify subacute compression as a separate form of the disease, which can develop within 2 to 14 days. The following pathological processes contribute to its appearance:
- Rupture of the intervertebral hernia.
- Growth of tumors or metastases.
- Formation of an abscess (purulent cavity).
As a rule, various neoplasms with slow growth and progression lead to the chronic form of the disease. With this type of compression, clinical symptoms increase gradually, which significantly complicates the diagnosis.
The defeat of the nerve roots of the spinal cord (radiculitis) in the prevailing majority of cases is associated with such a pathology of the spine as osteochondrosis.
Clinical picture
It should be noted right away that the nature of the symptoms is influenced by the type of compression and the level of damage to the spinal cord and nerve roots. At the same time, the rate of clinical manifestations will directly depend on what kind of compression myelopathy is observed: acute, subacute or chronic.
The most severe form of compression manifests itself. Flaccid paralysis, loss of all types of sensitivity, disruption of the normal functioning of internal organs - all this develops at the same time. This condition is called spinal shock. Over time, flaccid paralysis changes to spastic. Pathological reflexes, convulsions and contractures of the joints due to muscle spasm (a sharp restriction in mobility) are recorded. Some features of clinical symptoms in chronic compression myelopathy, depending on the level of the lesion:
- Cervical department. There are not intense pains in the occiput, neck and upper shoulder girdle. Skin sensitivity is impaired (numbness, tingling, etc.). Then there is weakness in the arms. Muscle tone suffers, their atrophy appears.
- Chest section. At this level, compression is rare. Nevertheless, if it occurs, then there will be a violation of the motor activity of the legs, a disorder of various types of sensitivity in the trunk region. There is a malfunction in the work of internal organs.
- Lumbar region. Chronic compression leads to dull muscle pain in the area of the lower extremities. In addition, skin sensitivity is impaired. Over time, weakness increases, tone decreases, and atrophy of the leg muscles occurs. The work of the pelvic organs is impaired (urinary incontinence, problems with the act of defecation, etc.).
With compression myelopathy at any level of the lesion (cervical, thoracic or lumbar spine), clinical symptoms are observed, indicating a violation of the functioning of internal organs.
Diagnostics

The appearance of the characteristic symptoms of movement disorders and sensory disorders allows an experienced doctor to suspect that, most likely, we are talking about diseases of the spinal cord. To date, computed and magnetic resonance imaging are considered the best diagnostic method for detecting compression myelopathy. The resolving power of these methods makes it possible to identify both the exact cause of the compression of the spinal cord and nerve roots, and to assess their current state.
If for some reason it is impossible to conduct a tomography, then an X-ray examination is prescribed. This method makes it possible to determine the cause of the compression based on the condition of the spine. X-ray images clearly show a fracture, dislocation of the vertebrae, intervertebral hernia, signs of degenerative-dystrophic diseases (osteochondrosis, spondyloarthrosis, etc.).
If necessary, a lumbar puncture is performed to analyze the cerebrospinal fluid. Also, myelography can be involved - this is an x-ray using a contrast agent that is injected into the cavity between the meninges.
Treatment
Acute and subacute forms of compression myelopathy require emergency surgery. Treatment consists in eliminating the cause of the spinal cord injury. With chronic compression, as a rule, elective surgery is performed.
If chronic compression of the spinal cord is associated with osteochondrosis, then a complex treatment consisting of several stages can be recommended. They start with conservative therapy, which will include:
- Taking non-steroidal anti-inflammatory drugs, chondroprotectors, vitamins and other drugs.
- The use of special corsets.
- Passage of courses of physiotherapy exercises, massage and physiotherapy.
If the conservative approach does not give the desired result or the progression of the clinical picture of the disease is observed, they resort to surgical treatment. The following types of surgical intervention can be used to help eliminate the factors that provoke spinal cord compression:
- Removal of intervertebral joints.
- Removal of the arches of the vertebrae.
- Elimination of intervertebral hernia.
- Replacing a damaged disk.
- Removal of hematoma, abscess, cyst, etc.
A highly qualified specialist should supervise the treatment of any spinal cord disease.
Myelitis
An inflammatory disorder of the spinal cord is called myelitis. This pathology is considered quite dangerous, since often after it, patients receive various groups of disabilities. It should be noted right away that myelitis is not a disease that goes away without a trace. Severe cases can even be fatal.
Causes
Risk factors for the development of myelitis are reduced immunity and severe hypothermia. The causes of the disease can be not only infectious agents. What can provoke inflammatory process in the spinal cord:
- Infection (viruses, bacteria, etc.).
- Injury.
- Poisoning with mercury, lead, etc. (toxic myelitis).
- Reaction to certain vaccines.
- Radiation therapy.
Clinical picture

Myelitis will be characterized by an acute or subacute course. General symptoms of inflammation are observed, such as a sharp rise in temperature, a feeling of weakness, fatigue, headaches, aching muscles and joints. Neurological symptoms begin with mild pain and numbness in the trunk (back, chest) and legs. Then, over the course of several days, symptoms of motor, sensory and autonomic disorders appear and intensify. Features of the clinical picture, given the level of damage:
- Cervical department. Flaccid paralysis of the hands is observed. In this case, the lower limbs are affected by spastic paralysis. Myelitis in the upper cervical segments is characterized by lesions of the arms and legs in the form of spastic paralysis, and there will also be impaired breathing and cardiac activity. All kinds of sensitivity suffer.
- Chest section. The inflammatory process at this level leads to the appearance of spastic paralysis of the lower extremities, seizures, pathological reflexes. The work of the pelvic organs is disrupted (urinary, the act of defecation). In addition, sensitivity disorder is always observed.
- Lumbar region. Peripheral paresis or paralysis of both lower extremities develops. Muscle strength and tone are noticeably reduced, deep reflexes drop out. Dysfunctions of the pelvic organs are noted in the form of an inability to control urination and the act of defecation (true incontinence).
As a rule, even after the treatment of myelitis, paresis and paralysis of those limbs that were affected remain. Since movement disorders are restored rather slowly.
Diagnostics

The characteristic clinical picture of the inflammatory process in the spinal cord gives a good reason to make a preliminary diagnosis of myelitis. To confirm the conclusion, a lumbar puncture is performed, which allows a detailed examination of the cerebrospinal fluid.
The nature of the damage and the assessment of healthy nerve structures can be performed using magnetic resonance imaging.
Treatment
All patients with signs of myelitis are admitted to the neurological department. Priority measures for treatment depend on the cause that triggered the development of the inflammatory process in the spinal cord. The following therapeutic methods can be applied:
- For non-infectious myelitis, glucocorticosteroids are prescribed medications(prednisolone, hydrocortisone, etc.) in shock doses. As the condition improves, the dosage of drugs is gradually reduced.
- For bacterial myelitis, antibiotics are used in the maximum allowable dosage.
- To relieve increased muscle tone, Seduxen, Melliktin or Mydocalm are used.
- To prevent the development of cerebral edema, diuretics are used (Furosemide, Lasix).
- In case of impaired urinary function, bladder catheterization is performed. A special tube is inserted to facilitate the passage of urine.
- Be sure to lubricate the skin with medicinal ointments or other means to prevent pressure ulcers.
- With severe intense pain, strong analgesics are used (Promedol, Tramadol, Fentanyl).
- B vitamins.
The rehabilitation program includes special physical exercise, massage sessions and physiotherapy procedures. The recovery period can take several years.
Tumors
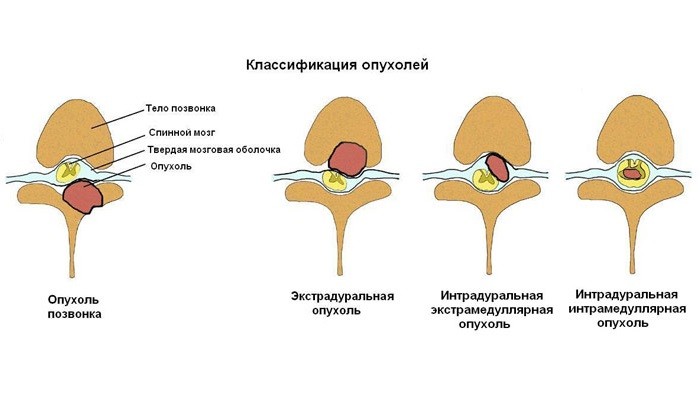
Regardless of the origin (nerve roots, membranes, vertebrae, etc.), location and nature of growth, tumors always lead to compression of the spinal cord. Statistics show that primary neoplasms are rarely diagnosed in children and people in old age. Meningiomas and neuromas account for more than 75% of all neoplasms of the spinal cord. There are two types of tumors:
- Extramedullary (provokes compression of nerve structures from the outside).
- Intramedullary (grow from the white or gray matter of the spinal cord itself).
Clinical picture
The location of the neoplasm and the nature of its growth will determine the clinical picture. An extramedullary tumor is initially characterized by pain syndrome associated with damage to the nerve roots. Then there is a slow progression of signs of spinal cord compression, manifested by paresis of the upper and / or lower extremities, sensory disturbances and disruption of the pelvic organs.
Intramedullary neoplasms are characterized by the appearance of clinical symptoms depending on the level of segmental lesions. For example, if the tumor process is located in the thoracic region, then there is intense girdle pain in the chest area, spastic paresis of the legs, sensory disturbance and problems with urinary excretion. Slow progression of neurologic symptoms over several months or years will be typical for this type of tumor.
The rapid development of symptoms (paresis, paralysis, loss of sensation, etc.) may be due to the tumor compressing the blood vessels that feed the central nervous system.
Diagnostics
To identify the cause of the spinal cord compression, standard diagnostic measures... In most cases, the following types of diagnostics are used:
- Radiography.
- Myelography (X-ray method with the introduction of a contrast agent).
- CT scan.
- Lumbar puncture.
- Magnetic resonance imaging.
Treatment

As a rule, they use surgery... The effectiveness of the surgical intervention depends on the type of neoplasm, its localization and the duration of the spinal cord compression. If there are justified suspicions of the presence of compression of the nerve structures, shock doses of glucocorticosteroids are urgently administered to reduce edema and preserve the function of the spinal cord.
Clinical experience shows that in case of extramedullary neoplasms, accompanied by a complete loss of motor, sensory and autonomic functions, it is possible to restore working capacity in a few months if the tumor is successfully removed. At the same time, neoplasms growing from the substance of the spinal cord are usually difficult to treat with surgery.
Radiation therapy is often used after surgery. If necessary, use symptomatic therapy (pain relievers, muscle relaxants, sedatives, etc.).
Spinal cord diseases often lead to irreversible neurological damage and persistent and severe disability. Pathological foci of insignificant size cause the occurrence of tetraplegia, paraplegia and impaired sensitivity downward from the focus, since almost all efferent motor and afferent sensory pathways pass through a small cross-sectional area of the spinal cord. Many diseases, especially those accompanied by external compression of the spinal cord, are reversible, and therefore acute lesions of the spinal cord should be classified as one of the most critical emergencies in neurology.
The spinal cord has a segmental structure and innervates the limbs and trunk. 31 pairs depart from him spinal nerves, which makes anatomical diagnosis relatively simple. Determining the localization of the pathological process in the spinal cord allows the border of sensitivity disorders, paraplegia and other typical syndromes. Therefore, in diseases of the spinal cord, a thorough examination of the patient is required with the use of additional laboratory tests, including NMR, CT, myelography, CSF analysis and study of somatosensory evoked potentials. Due to its ease of conduct and better resolution, CT and NMR are replacing standard myelography. NMR provides especially valuable information about the internal structure of the spinal cord.
Correlation of the anatomical structure of the spinal column and spinal cord with clinical symptoms
The universal organization of the longitudinal axis of the spinal cord according to the somatic principle makes it easy to identify syndromes caused by damage to the spinal cord and spinal nerves (see Ch. 3, 15, 18). Longitudinal localization of the pathological focus is established along the uppermost border of sensory and motor dysfunction. Meanwhile, the relationship between the vertebral bodies (or their superficial landmarks, spinous processes) and the spinal cord segments located below them complicates the anatomical interpretation of the symptoms of spinal cord diseases. Spinal cord injury syndromes are described according to the segment involved, rather than the adjacent vertebra. During embryonic development, the spinal cord grows more slowly than the spinal column, so that the spinal cord ends behind the body of the first lumbar vertebra, and its roots take a more vertical descending direction in order to reach the structures of the limbs or internal organs innervated by them. A useful rule of thumb is. that the cervical roots (with the exception of CVIII) leave the spinal canal through the holes above the corresponding vertebral bodies, while the thoracic and lumbar roots - under the vertebrae of the same name. The upper cervical segments lie behind the vertebral bodies with the same numbers, the lower cervical segments are one segment above their corresponding vertebra, the upper thoracic segments are two segments higher, and the lower thoracic segments are three. The lumbar and sacral segments of the spinal cord [(the latter form the conus medullaris)] are located behind the ThIX - LI vertebrae. To clarify the distribution of various extramedullary processes, especially in spondylosis, it is important to carefully measure the sagittal diameters of the spinal canal. Normally, at the cervical and thoracic levels these indicators are 16-22 mm; at the level of the vertebrae LI-LIII - about 15-23 mm and below - 16-27 mm.
Clinical syndromes of spinal cord diseases
The main clinical symptoms of spinal cord injury are loss of sensitivity below the border that runs along a horizontal circle on the trunk, that is, the "level of sensitivity disorders", and weakness in the limbs, innervated by descending cortico-spinal fibers. Sensory disturbances, especially paresthesias, may appear in the feet (or one foot) and spread upward, initially giving the impression of polyneuropathy, before a permanent boundary is established for sensitivity disorders. Pathological foci leading to a break in the cortico-spinal and bulbospinal tracts at the same level of the spinal cord cause paraplegia or tetraplegia, accompanied by an increase in muscle tone and deep tendon reflexes, as well as Babinsky's symptom. A detailed examination usually reveals segmental disorders, for example, a band of changes in sensitivity near the upper level of conductive sensory disorders (hyperalgesia or hyperpathy), as well as hypotension, atrophy, and isolated loss of deep tendon reflexes. The level of conduction disorders of sensitivity and segmental symptoms roughly indicate the localization of the transverse lesion. An accurate localizing sign is pain felt along the midline of the back, especially at the thoracic level; pain in the interscapular region may be the first symptom of spinal cord compression. Radicular pain indicates the primary localization of a spinal lesion located more laterally. With the involvement of the lower spinal cord - the cerebral cone, pain is often noted in the lower back.
In the early stages of an acute transverse lesion, the extremities may have hypotension rather than spasticity due to so-called spinal shock. This condition can persist for up to several weeks, and it is sometimes mistaken for an extensive segmental lesion, but later reflexes become high. In acute transverse lesions, especially those caused by infarction, paralysis is often preceded by short clonic or myoclonic movements in the limbs. Another important symptom of transverse spinal cord injury that requires close attention, especially when combined with spasticity and the presence of a level of sensory disorders, is autonomic dysfunction, primarily urinary retention.
Considerable efforts are being made to clinically distinguish between intramedullary (within the spinal cord) and extramedullary compression lesions, but most of the rules are approximate and do not reliably differentiate one from the other. The signs that testify in favor of extramedullary pathological processes include radicular pain; Brown-Séquard Half Spinal Syndrome (see below); symptoms of damage to peripheral motor neurons within one or two segments, often asymmetric; early signs of cortico-spinal tract involvement; a significant decrease in sensitivity in the sacral segments; early and pronounced changes in CSF. On the other hand, hardly localized burning pains, dissociated loss of pain sensitivity while maintaining musculo-articular sensitivity, preservation of sensitivity in the perineum, sacral segments, late arising and less pronounced pyramidal symptoms, normal or slightly altered CSF composition are usually characteristic of intramedullary lesions. "Intactness of sacral segments" means the preservation of the perception of pain and temperature irritations in sacral dermatomes, usually with SIII no SV. with rostral zones above the level of sensitivity disorders. As a rule, this is a reliable sign of intramedullary lesion, accompanied by the involvement of the most internal fibers of the spinothalamic pathways, but not affecting the outermost fibers that provide sensory innervation of the sacral dermatomes.
Brown-Séquard syndrome is a symptom complex of a half-transverse spinal cord lesion, manifested by homolateral monocle hemiplegia with loss of musculo-articular and vibration (deep) sensitivity in combination with contralateral loss of pain and temperature (surface) sensitivity. The upper limit of pain and temperature sensitivity disorders is often determined 1-2 segments below the site of spinal cord injury, since the fibers of the spinothalamic pathway, after the formation of a synapse in the posterior horn, pass into the opposite lateral cord, going up. If there are segmental disorders in the form of radicular pain, muscle atrophy, extinction of tendon reflexes, then they are usually unilateral.
Pathological foci, limited to the central part of the spinal cord or affecting mainly it, mainly affect the neurons of the gray matter and segmental conductors that intersect at this level. The most common processes of this kind are contusion with spinal cord injury, syringomyelia, tumors and vascular lesions in the basin of the anterior spinal artery. With the involvement of the cervical spinal cord, the syndrome of central spinal lesion is accompanied by weakness of the arm, which is much more pronounced in comparison with the weakness of the leg, and dissociated disorders of sensitivity (analgesia, i.e., loss of pain sensitivity with distribution in the form of a cape on the shoulders and lower part of the neck, without anesthesia, i.e. loss of tactile sensations, and with the preservation of vibration sensitivity).
Lesions localized in the body region C or below compress the spinal nerves that make up the cauda equina and cause flaccid asymmetric paraparesis with areflexia, which is usually accompanied by dysfunction of the bladder and intestines. The distribution of sensory disorders resembles the outline of a saddle, reaches the L level and corresponds to the zones of innervation of the roots included in the cauda equina. Achilles and knee reflexes are reduced or absent. Pain radiating to the perineum or thighs is often noted. With pathological processes in the area of the spinal cord cone, pain is less pronounced than with lesions of the cauda equina, and disorders of the functions of the intestines and bladder appear earlier; only Achilles' reflexes are dying out. Compression processes can simultaneously capture both the cauda equina and the cone and cause a combined syndrome of peripheral motor neuron lesions with some hyperreflexia and Babinsky's symptom.
The classic foramen magnum syndrome is characterized by muscle weakness in the shoulder girdle and arm, followed by weakness in the homolateral leg and, finally, in the contralateral arm. Volumetric processes of this localization sometimes give suboccipital pain that extends to the neck and shoulders. Horner's syndrome is another evidence of a high cervical lesion level, which is not observed in the presence of changes below the TII segment. Some illnesses can cause sudden "stroke-like" myelopathy without prior symptoms. These include epidural hemorrhage, hematomyelia, spinal cord infarction, prolapse of the nucleus pulposus, and subluxation of the vertebrae.
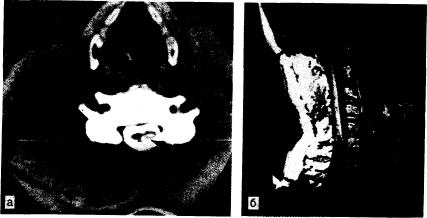
Spinal cord compression
Spinal cord tumors. Tumors of the spinal canal are divided into primary and metastatic and are classified into extradural ("epidural") and intradural, and the latter - into intra- and extramedullary (see Chapter 345). More common are epidural tumors originating from metastases in a nearby spinal column. Metastases from the prostate, mammary glands and lungs, as well as lymphomas and plasmacytic dyscrasias are especially often observed, although the development of metastatic epidural compression of the spinal cord is described in almost all forms of malignant tumors. The first symptom of epidural compression is usually local back pain, often worsening while lying down and causing the patient to wake up at night. They are often accompanied by radiating radicular pain that increases with coughing, sneezing and exertion. Pain and local tenderness on palpation often precede other symptoms for many weeks. Neurologic symptoms usually develop over days or weeks. The first manifestation of the syndrome of spinal cord injury is progressive weakness in the extremities, eventually acquiring all the signs of transverse myelopathy with paraparesis and the level of sensitivity disorders. With conventional radiography, destructive or blastomatous changes or a compression fracture at the level corresponding to the syndrome of spinal cord injury can be detected; radionuclide scans bone tissue are even more informative. CT, NMR and myelography remain the best imaging techniques for spinal cord compression. The area of horizontal symmetric expansion and compression of the spinal cord, compressed by an extramedullary pathological formation, is noticeable along the boundaries of the blockade of the subarachnoid space, usually with changes from the neighboring vertebrae (Fig. 353-1).
In the past, emergency laminectomies were considered necessary to treat patients with extramedullary spinal cord compression. However, the modern method of treatment with the introduction of high doses of corticosteroids and the rapid implementation of fractional radiation therapy turned out to be no less effective. The outcome often depends on the type of tumor and its radiosensitivity. Paraparesis often subsides within 48 hours of corticosteroid administration. In some incomplete early syndromes of transverse spinal cord injury, surgical treatment is more expedient, but in each case, an individual analysis of treatment tactics is required, taking into account the radiosensitivity of the tumor, the localization of other metastases and the general condition of the patient. But whatever treatment is chosen, it is advisable to carry it out quickly and prescribe corticosteroids immediately after spinal compression is suspected.
Intradural extramedullary tumors are less likely to cause spinal cord compression and develop more slowly than extradural pathological processes. Meningiomas and neurofibromas are more common; hemangiopericytomas and other enveloped tumors are quite rare. In the beginning, radicular sensory disorders and asymmetric neurological disorder syndrome usually occur. With CT and myelography, a characteristic picture of the dislocation of the spinal cord away from the outline of the tumor located in the subarachnoid space is visible. Primary intramedullary tumors of the spinal cord are discussed in Chapter 345.
Neoplastic compression myelopathies of all types initially lead to a slight increase in the protein content in the CSF, but with the onset of complete blockade of the subarachnoid space, the protein concentration in the CSF increases to 1000-10000 mg / L due to a delay in CSF circulation from the caudal sac into the intracranial subarachnoid space. Cytosis, as a rule, is low or absent, cytological examination does not reveal malignant cells, glucose content is within normal limits, if the process is not accompanied by widespread carcinomatous meningitis (see Chapter 345).
Epidural abscess. Patients with an epidural abscess respond to treatment but are often misdiagnosed early on (see Chapter 346). Furunculosis of the occipital region, bacteremia, as well as minor back injuries predispose to the occurrence of an abscess. An epidural abscess can develop as a complication of surgery or lumbar puncture. The reason for the formation of an abscess
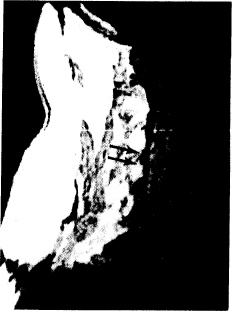
Rice. 353-1. Sagittal NMR view showing compression deformity of the TXII vertebral body by metastatic adenocarcinoma (under the arrows), as well as compression and displacement of the spinal cord. (Courtesy of Shoukimas G., M. D., Department of Radiology, Massachusetts General Hospital.)
Which, as it increases in size, compresses the spinal cord, serves as spinal osteomyelitis. The osteomyelitis lesion is usually small and often undetectable on conventional radiographs. During the period from several days to 2 weeks, the patient may have only unexplained fever and mild back pain with local tenderness on palpation; radicular pain appears later. As the abscess grows, it quickly compresses the spinal cord, and a syndrome of its transverse lesion appears, usually with a complete interruption of the spinal cord. In this case, rapid decompression by means of laminectomy and drainage is advisable, followed by antibiotic therapy prescribed on the basis of the results of cultivation of purulent material. Inadequate drainage often leads to the development of chronic granulomatous and fibrotic processes that can be sterilized with antibiotics, but which continue to act as a compression volumetric process. Purulent tuberculous abscesses, more common in the past, are still found in developing countries.
Spinal epidural hemorrhage and hematomyelia. Acute transverse myelopathy, which develops in minutes or hours and is accompanied by severe pain, can be caused by hemorrhage in the spinal cord (hematomyelia), subarachnoid and epidural space. The source of the latter is arteriovenous malformation or bleeding into the tumor during anticoagulant therapy with warfarin, but more often hemorrhages are spontaneous. Epidural hemorrhages can develop as a result of minor trauma, lumbar puncture, anticoagulant therapy with warfarin, and secondarily against the background of hematological diseases. Back pain and radicular pain often precede the onset of weakness for several minutes or hours and are so severe that patients are forced to take bizarre postures when moving. Epidural hematoma of lumbar localization is accompanied by the loss of knee and Achilles reflexes, whereas with retroperitoneal hematomas, only knee reflexes usually fall out. With myelography, a volumetric process is determined; on CT, changes are sometimes not detected, since the blood clot cannot be distinguished from the adjacent bone tissue. Blood clots can form as a result of spontaneous bleeding or be caused by the same factors as epidural hemorrhages, and in the subdural and subarachnoid spaces give a particularly pronounced pain syndrome. With epidural hemorrhage, CSF is usually clear or contains few red blood cells; with subarachnoid hemorrhage, the CSF is first bloody, and later acquires a pronounced yellow-brown tint due to the presence of blood pigments in it. In addition, pleocytosis and a decrease in glucose concentration can be detected, which gives the impression of bacterial meningitis.
Acute disc protrusion. Herniated discs in the lumbar spine are a fairly common pathology (see Chapter 7). Protruded discs of the thoracic or cervical vertebrae are less likely to cause compression of the spinal cord and usually develop after a spinal injury. Degeneration of cervical intervertebral discs with contiguous osteoarthritic hypertrophy causes subacute spondylitis-compression cervical myelopathy, discussed below.
Arthritic diseases of the spine are manifested in two clinical forms: compression lumbar spinal cord or cauda equina as a result of ankylosing spondylitis, compression of the cervical segments during destruction of the cervical apophyseal or atlantoaxial joints in rheumatoid arthritis... Spinal cord complications arising as one of the components of generalized joint damage in rheumatoid arthritis are often overlooked. Anterior subluxation of the bodies of the cervical vertebrae or atlas relative to the second cervical vertebra(CII) can lead to devastating and even fatal acute spinal cord compression following minor trauma such as whiplash or chronic compression myelopathy similar to that of cervical spondylosis. Separation of the odontoid process from the CII can cause a narrowing of the upper part of the spinal canal with compression of the cervicomedullary junction, especially during flexion movements.
Non-compression neoplastic myelopathy
Intramedullary metastases, paracarcinomatous myelopathy and radiation myelopathy. Most of myelopathies in malignant diseases are compressional. However, if the block cannot be detected with radiological examinations, it is often difficult to distinguish between intramedullary metastases, paracarcinomatous myelopathy and radiation myelopathy. In a patient diagnosed with metastatic cancer and progressive myelopathy, the non-compression character of which was confirmed by myelography. CT or NMR, most likely intramedullary metastasis; less often in such a situation occurs paraneoplastic myelopathy (see Chapter 304). Back pain most often serves as the first, although not mandatory, symptom of intramedullary metastasis, followed by increasing spastic paraparesis and, somewhat less often, paresthesia. Dissociated loss of sensitivity or its intactness in the sacral segments, more characteristic of internal than external compression, is rarely observed, while asymmetric paraparesis and partial loss of sensitivity are the rule. Myelography, CT and NMR show an edematous spinal cord without signs of external compression: in almost 50% of patients, CT and myelography give a normal picture; NMR is more effective in differentiating a metastatic focus from a primary intramedullary tumor (Fig. 353-2). Intramedullary metastases usually arise from bronchogenic carcinoma, less often from breast cancer and other solid tumors (see Chapter 304). Metastatic melanoma rarely causes external compression of the spinal cord and usually occurs as an intramedullary volumetric process. Pathologic metastasis is a single eccentrically located node resulting from hematogenous dissemination. Radiation therapy is effective in appropriate circumstances.
Carcinomatous meningitis, a common form of CNS lesion in cancer, does not cause myelopathy unless there is widespread subpial infiltration from the adjacent roots, resulting in nodules and secondary compression or infiltration of the spinal cord.
Rice. 353-2. Sagittal NMR image of the fusiform expansion of the cervical spinal cord with intramedullary tumor.
The tumor manifests itself as low density signals (indicated by arrows). (Courtesy of Shoukimas G., M. D., Department of Radiology, Massachusetts General Hospital.)
Incomplete, not accompanied by pain, cauda equina syndrome can be caused by carcinomatous infiltration of the roots (see Chapter 345). Patients often complain of headaches, and repeated CSF tests eventually reveal malignant cells, increased protein levels, and, in some cases, decreased glucose levels.
Progressive necrotizing myelopathy, combined with mild inflammation, occurs as a long-term effect of cancer, usually in solid tumors. The myelographic picture and CSF are usually normal, and there may be only a slight increase in the protein content in the cerebrospinal fluid. Subacute progressive spastic paraparesis develops over several days or weeks and is usually asymmetric; he is accompanied by paresthesia in distal parts limbs extending upward to the formation of the level of sensory disorders, and later - bladder dysfunction. Several adjacent spinal cord segments are also affected.
Radiation therapy causes distant subacute progressive myelopathy due to microvascular hyalinization and vascular occlusion (see Chapter 345). It often presents a serious differential diagnostic problem when the spinal cord is within the area exposed to radiation in order to treat other structures, for example, the lymph nodes of the mediastinum. The distinction between paracarcinomatous myelopathy and intramedullary metastasis is difficult, except in cases where there is clear evidence of previous radiation therapy in the anamnesis.
Inflammatory myelopathy
Acute myelitis, transverse myelitis, and necrotizing myelopathy. This is a group of related diseases, which are characterized by internal inflammation of the spinal cord and a clinical syndrome that develops within a few days to 2-3 weeks. It is possible to form a syndrome of complete transverse spinal lesion (transverse myelitis), as well as partial variants, including posterior columnar myelopathy with ascending paresthesias and a level of loss of vibration sensitivity; ascending, mainly spinothalamic disorders; Brown-Séquard syndrome with paresis of the leg and contralateral sensory disorders of the spinothalamic type. In many cases, the reason is viral infection... Most often, transverse myelitis is manifested by back pain, progressive paraparesis and asymmetric ascending paresthesias in the legs, later the hands are also involved in the process, and therefore the disease can be mistaken for Guillain-Barré syndrome. To exclude the compressive nature of the lesion, it is necessary to conduct radiological studies. In most patients, the CSF contains 5-50 lymphocytes per mm; sometimes more than 200 cells per 1 mm are found, occasionally polymorphonuclear cells predominate. The inflammatory process is more often localized in the middle and lower thoracic segments, but the spinal cord can be affected at almost any level. Chronic progressive cervical myelitis has been described, mainly in elderly women; this condition is considered as one of the forms of multiple sclerosis (see Ch. 348).
In some cases, necrosis is deep, it can grow intermittently for several months and involve the adjacent areas of the spinal cord; the latter decreases in size to a thin gliosis cord. This condition is denoted by the term "progressive necrotizing myelopathy". Sometimes the entire spinal cord is involved in the pathological process (necrotic panmyelopathy). If a transverse necrotic lesion occurs before or shortly after optic neuritis, then this condition is referred to as Devik's disease, or opticomyelitis. It seems that such processes are associated with multiple sclerosis, and many of them are variants of it. Systemic lupus erythematosus and other autoimmune diseases can also accompany myelitis. Post-infectious demyelinating processes usually have a monophasic course and only occasionally recur, but at the same time various symptoms are often observed, indicating the defeat of the same level of the spinal cord (see Chapter 347).
Toxic myelopathy. Toxic non-inflammatory myelopathy sometimes occurs simultaneously with optic nerve atrophy. It is more common in Japan and is due to the ingestion of iodochlorohydroxyquinoline. Most patients recover, but many of them persist with persistent paresthesias.
Arachnoiditis. This nonspecific term refers to inflammation, accompanied by cicatricial and fibrous thickening of the arachnoid membrane, which can lead to compression of the nerve roots and sometimes the spinal cord. Arachnoiditis is usually a postoperative complication or aftereffect from the introduction of radiopaque contrast agents, antibiotics, and harmful chemicals into the subarachnoid space. Soon after an adverse effect in the CSF, one may find big number cells and a high concentration of protein, but then the inflammatory process subsides. In the acute period, a slight fever is possible. The most pronounced bilateral asymmetric radicular pain in the extremities is also determined by signs of compression of the roots, for example, loss of reflexes. Back pain and radicular symptoms appear to be associated with lumbar arachnoiditis more often than they should; in addition, arachnoiditis is not a common cause of spinal cord compression (see Chapter 7). Treatment approaches are controversial; in some patients, improvement occurs after laminectomy. Multiple meningeal arachnoid cysts along the nerve roots can be a congenital anomaly. As these cysts grow larger, they cause deformation or stretching of the spinal nerve roots and ganglia, causing severe radicular pain in middle-aged people.
Spinal cord infarction
Since the anterior and posterior spinal arteries in atherosclerosis usually remain intact and are only rarely affected by angiitis or embolism, most spinal cord infarctions are the result of ischemia against the background of distant arterial occlusions. Aortic thrombosis or dissection causes spinal infarction by blocking the radicular arteries and stopping direct arterial blood flow to the anterior and posterior spinal arteries. A heart attack usually develops in the area of adjacent blood supply to the thoracic spinal cord between the large spinal branch of the aorta, the Adamkevich artery from below and the anterior spinal artery from above. Syndrome of anterior spinal artery disease usually occurs suddenly, apoplectiform, or is formed in the postoperative period as a result of clamping of the proximal aorta. However, in some patients, symptoms increase within 24-72 hours, which makes it difficult to make a diagnosis. There are isolated reports of spinal infarction in systemic arteritis, immune reactions in serum sickness and after intravascular administration of contrast medium; in the latter case, severe back pain during injection is a precursor.
A cerebral infarction caused by microscopic fragments of a herniated disc, the contents of which is the nucleus pulposus, can develop after a minor injury, often received during sports. At the same time, acute local pain is noted, alternating with rapidly advancing paraplegia and the syndrome of transverse spinal cord injury, which develops within a few minutes to an hour. In small intramedullary vessels and often inside the bone marrow of the adjacent vertebral body, pulp tissue is found. The path of its penetration from the disc material into Bone marrow and from there to the spinal cord remains unclear. This condition should be suspected in young people with transverse spinal cord injury syndromes as a result of an accident.
Spinal cord vascular malformation
Arteriovenous malformation (AVM) of the spinal cord is the most difficult pathological process to diagnose, which is explained by its inherent clinical variability. In its manifestations, it can resemble multiple sclerosis, transverse myelitis, spinal stroke, neoplastic compression. AVMs are more often localized in the lower thoracic and lumbar spinal cord and occur in middle-aged men. In most cases, the disease begins to manifest itself as a syndrome of incomplete progressive lesion of the spinal cord, which can occur sporadically and subacutely, resembling multiple sclerosis and accompanied by symptoms of bilateral involvement of the cortico-spinal, spinothalamic pathways and posterior columns in various combinations. Almost all patients suffer from paraparesis and are unable to walk for several years. Approximately 30% of ballrooms may suddenly develop a syndrome of solitary acute transverse myelopathy as a result of hemorrhage that resembles acute myelitis; others have several severe exacerbations. Approximately 50% of patients complain of back pain or radicular pain, which causes intermittent claudication, similar to that of lumbar stenosis; sometimes patients describe an acute onset with sharp, localized back pain. Changes in the intensity of pain and the severity of neurological symptoms during exercise, in certain positions of the body and during menstruation helps the diagnosis. Noises under the AVM area are rarely heard, but one should try to detect them at rest and after physical exertion. Most patients have a slightly elevated CSF protein, and some have pleocytosis. Hemorrhages in the spinal cord and CSF are possible. With myelography and CT, lesions are detected in 75-90% of cases if the dorsal subarachnoid space is examined in the supine position of the patient. The anatomical details of most AVMs can be detected using selective spinal angiography, a procedure that requires a lot of experience.
The pathogenesis of myelopathy caused by AVM (which did not bleed) is not well understood. Apparently, it is based on a necrotic non-inflammatory process, accompanied by ischemia. Necrotizing myelopathy has been described in dorsal AVMs with severe progressive intramedullary lesion syndrome. Since any necrotic process in the spinal cord can be accompanied by neovascularization and thickening of the vessel walls, there are conflicting judgments about the pathological basis of this vascular malformation.
Chronic myelopathy
Spondylosis. This term refers to some similar degenerative changes in the spine, leading to compression of the cervical spinal cord and adjacent roots. The cervical form is found mainly in the elderly, more often in men. It is characterized by: 1) narrowing of the intervertebral disc spaces with the formation of hernias of the nucleus pulposus or protrusion of the annulus fibrosus; 2) the formation of osteophytes from the dorsal side of the vertebral bodies;
3) partial subluxation of the vertebrae and 4) hypertrophy of the dorsal spinal ligament and dorsolateral facet joints (see sheet 7). Bone changes are reactive in nature, but there are no signs of true arthritis. The most significant factor causing symptoms of spinal cord injury is the "spondylitis bar" formed by osteophytes growing from the dorsal surfaces of the adjacent vertebral bodies; these osteophytes give horizontal compression of the ventral surface of the spinal cord (Fig. 353-3, a and b). The growth of the "bar" in the lateral direction, accompanied by hypertrophic changes in the joints and its invasion of the neural openings, often leads to the appearance of radicular symptoms. The sagittal diameter of the spinal canal also decreases as a result of disc protrusion, hypertrophy or arching of the dorsal spinal ligament, especially during neck extension. Despite the fact that radiographic signs of spondylosis are often found in the elderly, only a few develop myelopathy or radiculopathy, which is often associated with congenital narrowing of the spinal canal. The first symptoms are usually neck and shoulder pain combined with limited movement; compression of the nerve roots is accompanied by radicular pain in the arm, more often extending to the CV-CVI segments. Compression of the cervical spinal cord causes slowly progressive spastic paraparesis, sometimes asymmetric, and often paresthesias in the feet and hands. In most patients, vibration sensitivity in the lower extremities is significantly reduced, sometimes the border of vibration sensitivity in the upper part of the chest is determined. Coughing and straining often cause weakness in the legs and radiating pain in the arms or shoulder. Loss of sensitivity in the segmental zones on the arms, atrophy of the muscles of the hands, an increase in deep tendon reflexes on the legs and an asymmetric Babinsky symptom are often found. With an advanced pathological process, an imperative urge to urinate or urinary incontinence appears. Reflexes on the hands are often reduced, especially from the biceps muscles of the shoulders, which corresponds to the compression of the spinal segments of CV-CVI or the involvement of the same roots in the pathological process. The clinical picture is dominated by radicular, myelopathic or combined disorders. This diagnosis should be assumed in cases of progressive cervical myelopathy, paresthesias in the feet and hands, and atrophy of the muscles of the hands. Spondylosis is also one of the most common causes of difficulty walking in the elderly, as well as an unexplained increase in tendon reflexes from the lower extremities and Babinsky's reflexes.
Radiographs reveal spondylytic "beams", narrowing of the intervertebral clefts, subluxations, transformation of the normal curvature of the cervical spine and a decrease in the sagittal diameter of the canal to 11 mm or less, or to 7 mm with neck extension (see Fig. 353-3, a). CSF is usually normal or slightly high in protein. The study of somatosensory evoked potentials, which reveals a normal conduction velocity along large peripheral sensory fibers and a delay in central conduction in the middle and upper cervical segments of the spinal cord, is highly indicative.
Cervical spondylosis is diagnosed quite often. Many patients with lesions
Rice. 353-3. Radiographs of the cervical spine. a - lateral radiograph of the cervical spine, demonstrating the formation of a spondylitis "crossbar" as a result of joining adjacent osteophytes of the vertebrae CVI - CVII (shown by arrows); b - horizontal CT projection of the same patient at the level of the CVI vertebra after instillation of a water-soluble contrast agent into the subarachnoid space. The osteophytic process compresses and deforms the spinal cord (shown by arrows). (Courtesy of Shoukimas G 'M. D., Department of Radiology, Massachusetts General Hospital.).
Spinal cord lesions, especially with amyotrophic lateral sclerosis, multiple sclerosis and subacute associated degeneration, perform cervical laminectomy due to the fact that spondylosis is considered the cause of the existing disorders. Often after this procedure, there is a temporary improvement, which suggests a partial significance of spondylolytic compression, but soon myelopathy due to the underlying cause begins to progress again. On the other hand, mild progressive disturbances in gait and sensitivity may be mistakenly attributed to polyneuropathy.
With a mild course of the disease, rest and immobilization of the cervical spine with a soft corset are effective, in other cases traction is indicated. Surgical intervention is recommended for those patients who develop severe walking disorders, significant weakness in the hands or dysfunction of the bladder, or in the presence of an almost complete spinal block (according to myelography and CT).
Lumbar stenosis (see also Chapter 7) is intermittent chronic compression of the cauda equina, usually caused by congenital narrowing of the spinal canal at the lumbar level, which is exacerbated by disc protrusion and spondylitis. Physical activity provokes dull pain in the buttocks, thighs and calves, usually spreading along the way sciatic nerve; these pains subside at rest, and therefore resemble intermittent claudication of vascular genesis. At the height of pain, compared with the state of rest, a decrease in deep tendon reflexes and sensitivity is determined, while when examining the vessels, no changes are found. Lumbar stenosis and cervical spondylosis are often combined with each other, and the first, apparently, causes the periodic presence of fasciculations in the lower extremities with cervical spondylosis.
Degenerative and hereditary myelopathy. The prototype of hereditary diseases that cause spinal cord syndromes is Friedreich's ataxia, a progressive autosomal recessive disease characterized by ataxia of the lower extremities and trunk, which manifests itself in late childhood. There are also intentional tremors, awkwardness in the hands, and later - dysarthria. Kyphoscoliosis and pes cavus are common. Examination of the patient reveals areflexia, Babinsky's symptoms and gross disorders of vibrational and muscular-articular feelings. Fragmented and mild forms of the disease are also observed, occurring along with other syndromes, including spastic paraparesis (Strumpel-Lauren form), cerebellar cortical degeneration with ataxia, and olivopontocerebellar atrophy.
In patients with symmetric spastic paraparesis without sensory disorders, amyotrophic lateral sclerosis (motor neuron disease) can be assumed. It causes a pure syndrome of motor disorders with the simultaneous involvement of the cortico-spinal, cortico-bulbar pathways and cells of the anterior horns in the pathological process. Clinical and electromyographic signs of fasciculations and muscle denervation, suggesting motor neuron degeneration, support the diagnosis (see chapters 350 and 354).
Subacute combined degeneration with vitamin B12 deficiency. This treatable myelopathy causes progressive spastic and atactic paraparesis with polyneuropathy and usually with marked distal paresthesias in the feet and hands. Its possible occurrence must be borne in mind in cases resembling cervical spondylosis, late-onset degenerative myelopathy, and late-onset symmetrical spinal multiple sclerosis. The pathological process also involves peripheral and optic nerves as well as the brain. The diagnosis is confirmed by low vitamin B and serum levels and a positive Schilling test. This condition and alimentary degenerations close to it are considered in Ch. 349. There are conflicting opinions as to whether folate or vitamin E deficiency can lead to the development of a similar syndrome. In rare cases, multiple sclerosis and B12-deficient myelopathy are found in the same patient.
Syringomyelia. Syringomyelia is a progressive myelopathy, pathological characterized by the formation of cavities in the central part of the spinal cord. It is often idiopathic or a developmental anomaly (see Chapter 351), but can also be due to trauma, primary intramedullary tumors, external compression with central spinal necrosis, arachnoiditis, hematomyelia, or necrotizing myelitis. In the variant of the developmental anomaly, the process begins with the middle cervical segments and then spreads up to the medulla oblongata and down to the level of the lumbar spinal cord. Often, cavities are located eccentrically, which determines unilateral conduction symptoms or asymmetry of reflexes. In many cases, a combination with craniovertebral anomalies is observed, most often with an Arnold-Chiari anomaly, as well as with myelomeningocele, basilar impression (platybasia), atresia of the Magendie orifice and Dandy-Walker cysts (see Ch. 351).
The main clinical symptoms of syringomyelia resemble the syndrome of central lesion of the upper cervical spinal cord and are determined by the length of the pathological cavity and accompanying anomalies, for example, Arnold-Chiari. The classic manifestations include: 1) loss of sensation of the dissociated type (loss of pain and temperature while maintaining tactile and vibration) in the back of the neck, shoulders and upper extremities (distribution by the type of "cape" or "cape") with possible involvement of the hands; 2) muscle atrophy of the lower neck, shoulder girdle, upper limbs, hands with asymmetric loss of reflexes and 3) high thoracic kyphoscoliosis. More often, symptoms occur asymmetrically in the form of a one-sided decrease in sensitivity. In some patients, pain sensitivity in the face area decreases. which is caused by damage to the nucleus of the spinal tract of the trigeminal nerve at the level of the upper cervical segments. Cough-provoked headaches and neck pains are often observed in combination with Arnold-Chiari malformation.
In idiopathic cases, symptoms of the disease occur in adolescents or young adults and progress unevenly, often stopping in development for several years. Only a small number of patients do not become disabled, and more than half remain confined to a wheelchair. Analgesia contributes to the appearance of injuries, burns and trophic ulcers at the fingertips. In the advanced stages of the disease, neurogenic arthropathy (Charcot's joint) of the shoulder, elbow and knee joints often develops. Severe weakness in the lower extremities or hyperreflexia indicates a concomitant anomaly of the craniovertebral joint. Syringobulbia is the result of the expansion of the cavity to the level of the medulla oblongata and sometimes the bridge; usually the cavity is lateral
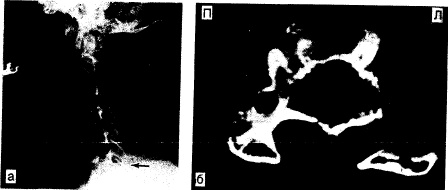
Rice. 353-4. A. Horizontal projection 1 hour after injection of a water-soluble contrast agent into the subarachnoid space shows the cervical spinal cord surrounded by contrast agent. This substance also fills a large intramedullary cystic cavity (shown by an arrow). B. On the sagittal NMR image of the same patient, the cystic cavity and the expansion of the cervical spinal cord are visible (shown by arrows). (Courtesy of Shoukimas G., M. D., Department of Radiology, Massachusetes General Hospital.)
Sections of the lining of the brain. Paralysis of the soft palate and vocal cord, dysarthria, nystagmus, dizziness, tongue atrophy and Horner's syndrome.
A slow increase in the cavity leads to a narrowing or complete blockage of the subarachnoid space. The cavities can be separated from the central channel, but are usually connected to it. The diagnosis is made on the basis of clinical signs and is confirmed by the detection of an enlarged cervical spinal cord with myelography, as well as by the results of CT scan performed several hours after the introduction of metrizamide or another water-soluble contrast agent into the subarachnoid space (Fig. 353-4, a). Best of all, cystic cavities are visible on NMR tomography (see Fig. 353-4, b). Due to the possibility of developmental abnormalities, additional examination of the cervico-medullary junction is necessary.
Treatment focuses on decompression of the cavity to prevent progressive damage and decompression of the spinal canal in the event of spinal cord expansion. When dilatation of the cervical spinal cord is combined with an Arnold-Chiari malformation, laminectomy and suboccipital decompression are indicated.
Tabes. Tabes and meningovascular syphilis of the spinal cord are rare these days, but they must be kept in mind in the differential diagnosis of most spinal cord syndromes. The most common symptoms of tabes spinal cord are typical transient and recurrent shooting pains, mainly in the legs and, somewhat less often, in the face, back, chest, abdomen and arms. In 50% of patients, gross ataxia of gait and legs appears, due to the loss of a sense of position. In 15-30% of patients, paresthesia, dysfunction of the bladder, acute abdominal pain and vomiting (visceral crises) are noted. The most characteristic symptoms of tabes dorsalis are the loss of reflexes from the lower extremities, disturbances in the sense of position and vibration sensitivity, a positive Romberg test, bilateral pupillary disorders, Argyll Robertson's symptom (absence of pupil constriction when illuminated while maintaining their reaction to accommodation).
Traumatic lesions of the spinal cord and its secondary compression in orthopedic pathology are discussed in the chapter on craniocerebral and spinal cord injuries (see Chapter 344).
General principles of caring for patients with acute paraplegia or tetraplegia
In the acute stages of paraplegia, primary importance is attached to the prevention of secondary urinary tract damage. There is an areflexia of the bladder with urinary retention, the patient does not feel its filling, and therefore there is a possibility of damage to m. detrusor due to its hyperextension. Urological rehabilitation measures include drainage of the bladder and prevention of urinary tract infections. This is best achieved by intermittent catheterization performed by trained personnel. Alternative methods are long-term drainage using a closed system, but associated with a fairly high incidence of infectious complications, as well as suprapubital drainage. Patients with acute lesions, especially those causing spinal shock, often require special cardiovascular therapy in connection with paroxysmal hypertension or hypotension, and it is necessary to administer solutions in order to correct deviations in circulating blood volume. Potential medical emergencies in patients with complete transverse spinal lesions are stress ulcers of the intestine and stomach. In such situations, therapy with cimetidine and ranitidine is effective.
Spinal cord lesions at a high cervical level cause mechanical respiratory failure of varying severity, requiring artificial ventilation. In case of incomplete respiratory failure with a forced vital capacity of 10-20 ml / kg, it is advisable to prescribe physiotherapy for the chest, and in order to relieve atelectasis and fatigue, especially when a massive lesion is located below the CIV level, a negative pressure corset can be used. In severe respiratory failure, tracheal intubation (if the spine is unstable, use an endoscope) followed by tracheostomy ensures that the trachea is accessible for ventilation and suction. A promising new method is electrical stimulation of the phrenic nerve in patients with localization of the pathological process at the Cy level or higher.
As the clinical picture stabilizes, it is necessary to pay attention to the psychological state of the patient and build a rehabilitation plan within the framework of real prospects. The vigorous program often gives good results in young and middle aged patients and makes it possible for them to return home to continue their normal life.
Some procedures can be performed by patients themselves with the help of others. Serious problems associated with immobilization: violation of integrity skin over areas of compression, urological sepsis and autonomic instability create the prerequisites for the occurrence of pulmonary embolism. The patient needs to frequently change the position of the body, use skin applications of emollients and soft bedding. The specially designed beds make it easier to turn the patient's body and a more even distribution of body weight without predominantly loading the bony protrusions. If the sacral segments of the spinal cord are preserved, then it is possible to achieve automatic emptying of the bladder. First, patients urinate reflexively in the intervals between catheterizations, and later learn to induce urination using various techniques. If the presence of residual urine volume may lead to infection, then surgical procedures or the placement of an indwelling catheter are necessary. Most patients need to monitor and empty their bowels at least twice a week to avoid bowel distension and obstruction.
Severe hypertension and bradykinesia occur in response to negative superficial stimuli, distension of the bladder or bowel, or surgical manipulation, especially in patients with damage to the cervical or upper thoracic segments of the spinal cord. Hypertension may be accompanied by severe redness and profuse sweating in areas above the level of the lesion. The mechanism of these autonomic disorders is not well understood. In this regard, the appointment of antihypertensive drugs is required, especially during surgery, but it is not recommended to use beta-blockers. In some patients, severe bradycardia occurs as a result of tracheal aspiration; this can be avoided with the introduction of small doses of atropine. A formidable complication in the early period is embolism pulmonary artery against the background of immobilization; it is noted in about 30% of patients after acute spinal cord injury.
Specialists identify combined, ischemic (myeloischemia) and hemorrhagic vascular diseases of the spinal cord. Also, these diseases include a variety of malformations. vascular system in the spinal cord region, such as vascular malformations and aneurysms.
Signs of vascular diseases of the spinal cord
Vascular diseases of the spinal cord can develop for a variety of reasons - due to acquired changes in the vascular wall, congenital vascular anomalies.
Types of violations
Acute spinal circulation disorder can manifest itself in a very diverse way, therefore, only a qualified doctor can recognize it after use. different methods diagnostics. In some cases, the causes of the onset of symptoms of these diseases may be congenital anomalies in the structure of the vessels of the capillary, venous or arterial bed - they may not appear for many years, and the reasons for their progression are different.
The manifestations of spinal cord infarction are diverse, since they directly depend on where the lesion is located. So, if there is a blockage of the anterior spinal cord, then there will be necrosis in the anterior part of the spinal cord. In this case, the patient subacutely or acutely develops lower spastic paraplegia, accompanied by dysfunction of the pelvic organs and impaired sensitivity. If the anterior spinal artery, located at the level of the cervical segments, is affected, flaccid arms and spastic paraparesis of the legs will appear, accompanied by dissociated temperature and pain para-anesthesia (that is, loss of sensitivity in symmetrical areas of the body) and dysfunction of the pelvic organs. In the event that the lesion occurred in the region of the lumbosacral segments, lower flaccid paraplegia will appear, accompanied by areflexia, dissociated paraanesthesia and disruption of the pelvic organs.
In any case, to clarify the cause of the pathology and the mechanism of its development, it is necessary to consult a qualified specialist (neurologist or neuropathologist), as well as perform a whole range of diagnostic procedures and laboratory tests.
Manifestations of pathology and their dependence on the types of violation
If there are any diseases of the spinal cord, the symptoms are likely to appear almost immediately. Such diseases are characterized, first of all, by loss of sensitivity in the area below the so-called "level of sensitivity disorders", which is accompanied by spasticity of the limbs and muscle weakness.
Sensory disturbances most often manifest as paresthesias developing in both feet or in one of them. In this case, paresthesia can spread upward. The level of vibration and pain sensitivity disorder, as a rule, coincides with the level of localization of the transverse lesion of the spinal cord.
Various autonomic dysfunctions are also characteristic of this kind of disease. First of all, the patient should be alerted by acute or progressive urinary retention, which is accompanied by spasticity and sensitivity disorder.

If there is a rupture of the corticospinal tract, then the patient will have quadraplegia or paraplegia, accompanied by increased muscle tone, increased tendon reflexes, and a positive Babinsky symptom. There are also segmental signs of the disease, which serve as a rough indicator of the level of damage.
One of the leading symptoms of this kind of disease is pain. , which are localized in the midline, help doctors determine the place where the lesion is localized. may signal compression of the spinal cord radiating to the lower back, then this symptom may indicate damage to the medullary cone, that is, the terminal part of the spinal cord.
If there is a lesion at the L4 level of the vertebra or below it, then the patient will develop asymmetric flaccid paraparesis, accompanied by dysfunction of the rectum and bladder, lack of reflexes, loss of sensitivity (starting from level L). As a rule, patients complain of pain that radiates to the thigh and perineum. With the defeat of the medullary cone, pain is not observed, but dysfunction of the rectum and bladder appears quite quickly. If a person simultaneously has compression injuries of the cauda equina and cone, then he will show signs of peripheral motoneurons, hyperreflexia, or a positive Babinsky symptom.
Extramedullary Disorders
Extramedullary lesions are characterized by symptoms such as asymmetric lower motor neuron lesions, Brown-Séquard syndrome, sacral sensory loss, and early corticospinal symptoms. If the lesion is localized at the Foramen magnum level, then the person will be disturbed by muscle weakness of the arm and shoulder, which is accompanied by ipsilateral, and then contralateral lesion of the leg, and later of the arm. If present, the doctor may assume that the cervical region is affected.
Intramedullary Disorders
But intramedullary lesions are usually accompanied by very burning pain. Moreover, it is rather difficult to determine the localization of unpleasant sensations. Also, the patient has a loss of pain sensitivity (while the sense of the position of the joint, sacral and perineal sensations remain) and mild corticospinal symptoms.
Signs of vascular diseases of the spinal cord in children

The clinic of the disease depends on how widespread the vascular pathology is along the diameter and length of the spinal cord, as well as on the level at which the lesion is localized.
Ischemia in the cervical spine in children will be manifested by weakness of both or only one of the arms, as well as a decrease in their muscle tone. If the child suddenly has weakness in both legs, then this may be a signal of a violation of the blood supply to the lumbar or thoracic level of the spinal cord. Sometimes weakness in the legs is accompanied by dysfunction of the pelvic organs, in particular, urinary dysfunction. Thus, it can be assumed that enuresis in some children may be of vascular origin.
Sometimes a feeling of weakness in the legs is observed in children only while walking. At the same time, stopping or resting significantly improves the well-being of the baby. This symptom is called intermittent spinal claudication.
Arteriovenous malformation is characterized by slow progression. The child gradually increases the feeling of weakness in the area of both legs, he is worried about pain in the spine, radiating to the legs, and sometimes disorders like "intermittent claudication".
In order to diagnose this kind of disease in a baby, you need to contact a qualified specialist. He will be able to determine what kind of diagnostic procedures a child needs to undergo in order to make him an accurate diagnosis. This can be computed tomography, analysis of cerebrospinal fluid and other methods of examination.
In patients, even the most early age it cannot be ruled out that malignant neoplasms may be hidden under the symptoms of vascular pathology. A timely examination will help to distinguish them - the tactics of treatment and the prognosis of these conditions are different, but in either case, timely therapy is necessary.
Treatment of vascular diseases of the spinal cord
Treatment of this kind of disease can only be carried out by a qualified doctor.... Attempts to self-medicate or the appointment of drug and other types of therapy before a diagnosis is made (at least preliminary) can provoke a sharp deterioration in the patient's well-being. When acute or rapidly progressing circulatory disorders in the vessels of the spinal cord are identified, it is possible to simultaneously carry out diagnostic procedures, analyzes and prescribe drugs that improve the patient's condition, regardless of his age.
What are the components of the treatment?
Drug treatment of this pathology involves the use of almost all groups of pharmacological drugs known to modern medicine. Medicines prescribed by a doctor can be prescribed both in the form of injections (mainly intramuscular or intravenous), and in the form of tablets (when the activity of the process subsides).
In any case, the therapy program should take into account:
- the use of drugs that improve microcirculation and collateral circulation, such as complamin, aminophylline, cavinton, nicotinic acid and dibazol;
- appointment diuretics medicines, for example, lasix;
- use of antiplatelet agents (for example, acetylsalicylic acid);
- the appointment of vitamins of group B and C.
Features of the therapy of some vascular pathologies of the SM
V recovery period various physiotherapy procedures can be prescribed, and. Often, in the treatment, drugs are used that can stimulate the conduction of nerve impulses (galantamine, proserin and others), as well as absorbable agents (cerebrolysin, aloe, and so on). Often, doctors use drugs that reduce muscle tone (Relanium, Elenium, Phenibut, and others).
In the event that the compression was caused by a tumor and the patient has epidural metastases, he is prescribed in order to reduce the edema, and radiation of the metastases is also carried out, but chemotherapy is not always used. If the tumor does not respond to this treatment, surgery is performed.
Operative treatment it is also required for spinal fracture or displacement (spinal injuries) - these pathologies are not vascular disorders, but circulatory disorders remain one of the mandatory components of this condition.
With an epidural, regardless of the reason for its development, an urgent surgical intervention is performed in order to drain it, as well as to obtain purulent material for bacteriological examination, which is necessary in order to prescribe suitable antibiotics. With hematomyelia (epidural hemorrhage), the clot is removed. The causes of dyscrasia, which led to hemorrhage, must be established and, if possible, eliminated. In this case, the appointment of drugs that affect the rheological properties and blood coagulability is shown (only under the control of a coagulogram).
It should be noted that spinal cord diseases should not be treated on their own. The fact is that this can only lead to an aggravation of the disease and the emergence of various complications... In order to avoid unpleasant consequences, it is recommended to consult a qualified neurologist as soon as possible. The prognosis of the disease depends on how extensive the lesion was and where it was located. As a rule, the earlier the correct treatment was started, the more favorable the prognosis will be. True, sometimes even with timely provision of medical care the patient still has persistent disorders of the sensory and motor spheres, movement disorders and other residual symptoms.
So, vascular diseases affecting the spinal cord can lead to very serious consequences. Therefore, people who find their symptoms in themselves should definitely consult a qualified doctor in order to undergo diagnosis and treatment. Inattention to one's own health, refusal to consult a doctor and non-compliance with his recommendations can cause disability in the patient.
By the way, you may also be interested in the following FREE materials:
- Free book "TOP-7 Harmful Exercises for Morning Exercises You Should Avoid"
- Reconstruction of the knee and hip joints with arthrosis- free video recording of the webinar, which was conducted by the doctor of exercise therapy and sports medicine - Alexander Bonin
- Free lessons on the treatment of lower back pain from a licensed exercise therapy doctor... This doctor has developed a unique system for the restoration of all parts of the spine and has already helped more than 2000 clients with various back and neck problems!
- Wondering how to treat a pinched sciatic nerve? Then carefully watch the video on this link.
- 10 essential nutrients for a healthy spine- in this report you will find out what the daily diet should be so that you and your spine are always in a healthy body and mind. Very useful information!
- Do you have osteochondrosis? Then we recommend to study effective methods lumbar, cervical and breast osteochondrosis without drugs.
Enter your e-mail to receive a free book "7 simple steps to a healthy spine "
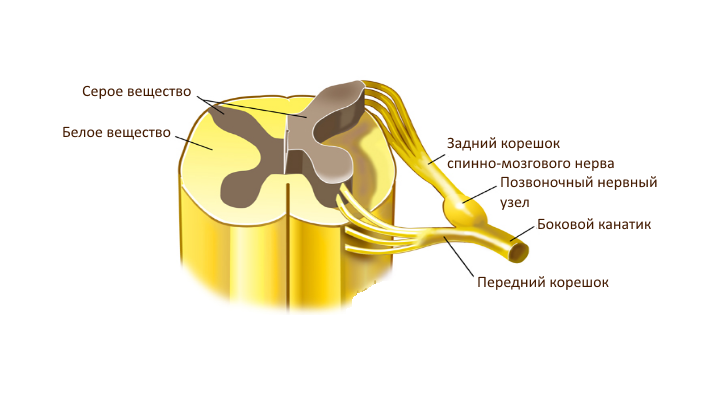
The spinal cord is an organ of the central nervous system, consisting of nerve cells and fibers and located in the spinal canal. It starts from the brain and ends in the vertebrae of the lumbar spine and is a long cord, shaped like a cylinder. It consists of gray matter surrounded by white matter on all sides. The gray matter is predominantly nerve cells, and the white matter is the processes of nerve cells. Spinal cord injury can be triggered by various factors. Diseases of the brain and spinal cord, as well as other lesions of its various parts, can cause sensory, motor and autonomic disorders.
The length of the spinal cord of an adult is from 41 to 45 cm. The spinal cord regulates the functions of the whole organism by transmitting nerve impulses to all internal organs.
Symptoms of damage to the human spinal cord and its various diseases are:
- motor disorders of the upper and lower extremities;
- pain in the neck and lower back;
- violation of skin sensitivity;
- frequent urination and urinary incontinence;
- paralysis and muscle atrophy;
- loss of joint-muscle sensitivity;
- local increase in skin temperature;
- pain in the muscles.
In the human spinal cord, 5 sections can be distinguished: cervical, thoracic, lumbar, sacral, coccygeal. Spinal cord injury syndromes differ at different levels, and also depending on which substance is affected, gray or white.
Spinal Cord Compression

They are a complex of neurological symptoms that are caused by the displacement and deformation of the spinal cord. This can occur when exposed to a pathological formation and when the vertebrae are displaced. Compression (squeezing) of the spinal cord affects its normal function.
Epidular abscess. A disease that is caused by infectious processes in the brain or spinal cord. It can be located in any part of the spinal canal. The reasons may be diseases such as otitis media, inflammation in the paranasal sinuses, osteomyelitis of the bones. The causative agents of this pathology include anaerobic flora, streptococci, staphylococci, salmonella, fungi and gram-negative bacilli. With complications, meningitis and meningoencephalitis can occur. To diagnose the disease, CT and MRI are performed. The main method of treatment is surgery (laminectomy, abscess removal) in combination with long-term antibiotic therapy with the appointment of large doses of antibiotics.
Hematomyelia. manifested by acute transverse myelopathy, accompanied by severe pain in back. It is rare, but can develop as a result of injuries (falling from a height, gunshot wound, electric shock, etc.), damage to the spinal vessels (due to fractures of the spine), arteriovenous malformations of the vessels of the spinal cord (thinning and rupture of the vessel walls). The manifestation of symptoms depends on the location. Development is possible at the level of the cervical spinal cord, thoracic segments, at the level of the lumbar thickening. Diagnosed with MRI. Treatment involves strict bed rest, local hyperthermia, and the use of hemostatic agents. In addition, it is necessary to carry out activities aimed at restoring the functions of the spinal cord.
Other indirect lesions. Spinal cord compression can be caused by arthritic diseases of the spine, proliferation of epidular adipose tissue in iatrogenic or primary Cushing's syndrome, and some hematological diseases.
Brain tumors
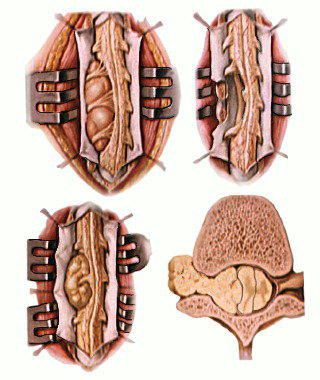 In the case of a pathological formation, it is not the structure and type of the tumor that matters, but the place of its localization. By origin and location, spinal cord cancers are classified as follows:
In the case of a pathological formation, it is not the structure and type of the tumor that matters, but the place of its localization. By origin and location, spinal cord cancers are classified as follows:
- Extradural. They are the most malignant, have a high growth rate and have a destructive effect on the spine. They grow from the tissues of the dura mater or the vertebral body. These include primary tumors of the spinal column, angiolipoma, chloroma, and metastatic tumors (cancers of the lungs, prostate, breast).
- Intradural. Extramedullary pathological formations localized under the dura mater (meningiomas, neurofibromas).
- Intramedullary. Pathological formations from clay tissue, located in the very substance of the spinal cord. These include astrocytomas and ependiomas.
To diagnose diseases of the human spinal cord and brain, neurosurgeons and oncologists perform neurological examination, radiography, MRI, CT. Most effective treatment spinal cord tumors is a surgical procedure. Conservative treatment can cause improvement and contribute to remission, but they are most often short-lived and incomplete.
In the treatment of malignant lesions of the spinal cord, X-ray therapy is additionally used, which delays tumor growth and helps to reduce many neuropathological symptoms.
Consequences of intervertebral hernias
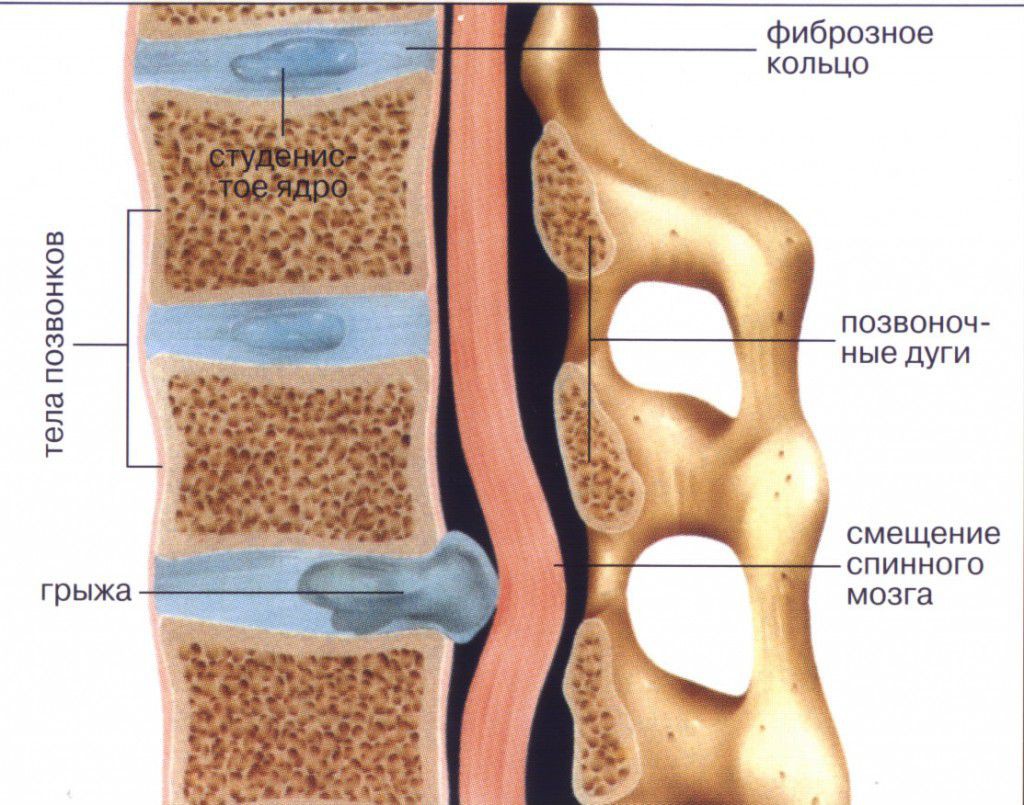
The rupture of the annulus fibrosus with a change in the location of the nucleus pulposus of the intervertebral disc causes the appearance of intervertebral hernias. Depending on the zone of their localization, the symptoms of the manifestation of hernias may be different.
The fact that intervertebral hernias of the spinal cord are involved can cause spinal dysfunction of the brain (myelopathy). As a result, the work of the vestibular apparatus, pelvic organs is disrupted, and weakness of the lower extremities is felt. In some cases, strong pressure on the spinal cord can lead to paralysis of the lower body.
The presence of hernias does not always cause complaints from the patient. Very often, there are no symptoms, which makes the identification of hernias very difficult and possible only after an MRI scan. However, the presence of hernias can cause serious problems in patients. Among them:
- back pain (starts from the buttocks and is localized in the back or side of the leg to the knee);
- pain in the leg (occurs after back pain);
- violation of sensitivity in the legs;
- feeling of weakness in the legs (especially in the knees and joints);
- disturbances in the work of the genitourinary sphere;
- numbness in the perineum.
For severe symptoms intervertebral hernias you should immediately contact a specialist, because often the causes of complications are the large sizes of hernias.
Risk factors for the occurrence of intervertebral hernias are smoking, overweight, high growth, activities associated with physical activity on the spine.
In most cases, it is non-surgical and involves the use of anti-inflammatory drugs, manual therapy, and strengthening exercises. Surgical treatment of hernias is indicated for dysfunctions of the spinal cord, with progressive neurological deficits, and if the patient is in severe pain.
Non-compression neoplastic myelopathy
Intramedullary metastases, radiation and paracarcinomatous myelopathy. When diagnosing, these diseases are very difficult to differentiate. The greatest likelihood of intramedullary metastasis, which is most often a consequence of bronchogenic carcinoma, less often - cancerous tumors (for example, breast). On CT and MRI, spinal cord edema with no signs of external compression is visible. Treatment is with radiation therapy.
Progressive necrotizing myelopathy. It affects several neighboring ones, is a long-term effect of solid cancers and is combined with mild inflammation. Patients develop progressive spastic paraparesis, characterized by asymmetry, parasthesia in the distal extremities, after some time, the functions of the pelvic organs are impaired.
Carcinomatous meningitis. The defeat of the central nervous system with cancers that occurs as a result of carcinoma and does not cause myelopathy if it does not spread and infiltrate from the adjacent roots, which as a result lead to infiltration of the spinal cord or the formation of nodules and secondary compression.
Melopathies and inflammation
Acute myelitis, transverse myelitis and necrotizing myelopathy are similar diseases in which the spinal cord becomes inflamed. The clinical syndrome develops from several days to several weeks. The most common cause is a viral infection. With myelitis, the patient complains of back pain and muscle weakness, which progresses rapidly. In addition, asymmetric ascending parasthesias in the legs are observed.
Infectious myelopathy. Spinal cord viral lesions are associated with specific types of myelitis. In the past, poliomyelitis, in which gray matter is affected, was the most common. Nowadays, the cause of viral lesions of the spinal cord is most often herpes zoster, less often - lymphotropic virus, HIV.
Arachnoiditis. Variety inflammatory disease the brain and spinal cord, in which the lesion occurs in the arachnoid membrane. The reasons can be transferred various acute and chronic infections, trauma, chronic intoxication, inflammatory diseases of the paranasal sinuses. During treatment, the first step is to eliminate the source of the infection. Antibiotics, pathogenetic therapy, metabolic therapy are prescribed.
Vascular diseases
Angioneurology is a branch of neurology that studies vascular diseases of the nervous system. Nowadays, this is one of the most important problems in medicine, since vascular diseases are the cause of death in 12-14% of all deaths. Angioneurologists attach great importance to the prevention of vascular diseases of the spinal cord at the level of studying the causes, developing new preventive methods.
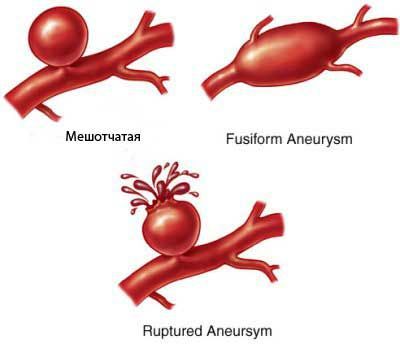
Types of aneurysms in blood vessels
Diseases can be caused by a pathological condition of the vessels that causes their damage, such as venous thrombosis, atherosclerosis, aneurysm, arterial dissection, lipo-hyalinosis, amyloid deposition. Diseases can develop if the viscosity of the blood is increased with insufficient blood flow, with a reduced perfusion pressure. In addition, a ruptured vessel may be the cause.
Vascular malformation of the spinal cord, AVM (arteriovenous malformation) of the spinal cord clinical picture may resemble transverse myelitis, multiple sclerosis, spinal stroke, neoplastic compression. Therefore, this disease is considered the most difficult to diagnose. There is paraparesis, progressive lesions of the spinal cord, radicular pain causing lameness, back pain.
Heart attack and its consequences
A heart attack occurs with an acute violation of the spinal circulation, in which the functions of the spinal cord are upset due to difficulties in the flow of blood. It can occur in almost any department, which is influenced by the reason why a heart attack develops.
It is often difficult to determine what exactly caused a heart attack, but most often this occurs as a result of blood clots in small vessels through which blood flows to the spinal cord, damage to the extravertebral arteries. Thus, spinal infarction causes thrombosis or dissection of the aorta. In addition, a heart attack can develop with arteritis, serum sickness.
Spinal cord infarction almost always affects several departments. Vessels suffer from obliterating thromboangiitis, nodular periarthritis. General ischemic infarction can very often be caused by impaired spinal circulation or discirculatory myeloischemia.
 A heart attack can develop even as a result of a minor injury (for example, received while playing sports). In this case, the infarction can be caused by microscopic particles of a herniated disc. How they get to the bone, and from there to the spinal cord, is unclear, but pulp tissue is often found in the vessels. Symptoms of the lesion that determine a heart attack are characterized by sudden severe back pain, decreased pain and temperature sensitivity, bilateral flaccid paresis of the extremities. Spinal infarction at the time of its development can cause headache, nausea, fainting, a state of general weakness.
A heart attack can develop even as a result of a minor injury (for example, received while playing sports). In this case, the infarction can be caused by microscopic particles of a herniated disc. How they get to the bone, and from there to the spinal cord, is unclear, but pulp tissue is often found in the vessels. Symptoms of the lesion that determine a heart attack are characterized by sudden severe back pain, decreased pain and temperature sensitivity, bilateral flaccid paresis of the extremities. Spinal infarction at the time of its development can cause headache, nausea, fainting, a state of general weakness.
Heart attacks most often occur in people between the ages of 50 and 60. In patients under the age of 40, myocardial infarction is most often caused by vasculitis, aortic pathologies, chronic perimedullary process, and in older people - by aortic pathologies.
Spinal cord diseases (myelopathy)A heart attack is diagnosed using MRI. Treatment in most cases is symptomatic.
Clinical neuroanatomy
Figure 1 shows a cross-section of the spine showing the location of the main pathways of neurotransmission. The main conducting motor pathway - the corticospinal tract originates in the opposite hemisphere, subsequently most of the fibers pass to the opposite side. Similarly, the spinothalamic tract crosses, transmitting sensory information from the opposite side of the body, while the posterior columns transmit ipsilateral information about the position of body elements in space and the feeling of vibration.
Rice. one.
Symptoms of defeat
Due to the distribution of most of the pathways in the spinal cord, most patients usually have a combination of motor, sensory and autonomic disorders.
Movement disorders
Most patients show symptoms of damage to the central motor neuron of both legs ( spastic paraparesis) or with damage to the upper cervical spine of all four limbs ( spastic tetraparesis). Damage to the cervical spinal cord can lead to the development of lower spastic paraparesis in combination with mixed symptoms of damage to the central and peripheral motor neurons in the upper limbs due to the simultaneous damage to the pathways and roots in cervical spine spinal cord.
Sensitivity disorders
A sign of spinal cord injury is the presence of the level of sensitivity disorders, for example, on the trunk, skin sensitivity is impaired below a certain level, and above it is normal. In a patient with spastic paraparesis desensitization level represents a certain value for confirming the presence of a spinal cord lesion, but the diagnostic significance of this sign is limited precisely by the anatomical localization of the lesion. Thus, the level of sensory impairment in the Th10 segment does not always indicate a lesion directly at Th10, but, rather, a lesion at or above Th10. This is essential in clinical practice. For example, when examining by neuroimaging methods of a patient with acute spinal cord compression, which requires urgent treatment, and the sensitivity level at Th10 (the imaging area is limited to the thoracic region), underlying lesions that are amenable to surgical treatment may not be detected.
Vegetative disorders
Bladder involvement is an early sign of spinal cord injury, with patients complaining of urgency and frequent incontinence. Gastrointestinal symptoms are less common in the early stages of the disease, although patients may complain of stool incontinence. Sexual dysfunction, in particular erectile dysfunction, is also common.
Other manifestations of spinal cord injury include pain in the neck or lower back, or indications of an injury.
Specific spinal syndromes
Syndromes of extramedullary and intramedullary lesions
External compression of the spinal cord - extramedullary lesion (tumor or prolapsed intervertebral disc), causes loss of sensitivity in the sacral dermatomes ( saddle anesthesia). The reason for this is that the part of the spinothalamic tract closest to the surface of the spinal cord (transmitting information from the lumbosacral dermatomes) is most vulnerable to external compression (Fig. 2). In case of internal (intramedullary) lesion, on the contrary, the fibers located in the center of the spinothalamic tract are primarily affected, while the fibers from the sacral region remain intact for a certain time ( sacral release), although this is not a strict rule (Fig. 2).
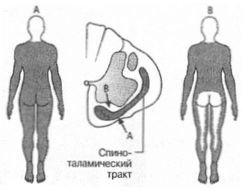
Rice. 2. Extra- and intramedullary spinal cord injury. The location of the pathways in the spinothalamic tract is shown - the fibers from the sacral dermatomes (S) are located most laterally, followed by the fibers from the lumbar (L), thoracic (T), and, most centrally, from the cervical dermatomes. External compression (A) is accompanied by damage to fibers from sacral dermatomes, while in intramedullary damage (B) these fibers may remain intact
With unilateral damage to the spinal cord, a characteristic syndrome of motor and sensory disorders develops. In its most complete form, which occurs with complete unilateral damage to the spinal cord, this condition is called Brown-Séquard syndrome (Fig. 3). This case is precisely the situation in which the level of impairment of sensitivity does not provide accurate information about the location of the lesion.

Rice. 3. Brown-Séquard syndrome. Damage to the central motor neuron on the side of the same name (since the descending corticospinal pathways have already crossed in the medulla oblongata). Loss of deep sensitivity and a sense of vibration is also observed on the side of the same name in relation to the lesion (due to the fact that the fibers rising in the posterior columns do not intersect until they reach the medulla oblongata). Loss of pain and temperature sensitivity is observed on the side opposite to the lesion focus (since the pathways intersect in the spinal cord at the level of the roots entering the spinal cord or slightly higher). It is also possible a strip of hypesthesia (sometimes in combination with spontaneous pain) at the level of the lesion due to damage to fibers that have not yet crossed in the contralateral spinothalamic tract
A rare condition in which a cavity filled with CSF forms in the spinal cord ( syrinx - reed) (fig. 4). It is manifested by the development of a characteristic motor and sensory neurological deficit (Fig. 5). Usually, at first, the cavity develops in the lower cervical spinal cord, over time it can spread throughout the longitudinal axis of the spinal cord. Patients develop lower spastic paraparesis with signs of peripheral motor neuron damage in the upper extremities (due to damage to both the corticospinal tract and the anterior horns of the cervical spinal cord). Deep sensitivity, the conducting fibers of which are located in the posterior columns of the spinal cord, is usually preserved, while pain sensitivity is impaired due to the defeat of the crossing fibers in the area of the cavity ( dissociated anesthesia). Loss of superficial (pain and temperature) sensitivity usually spreads like a "jacket" - anesthesia zones with upper and lower levels determined by the volume of the cavity. In some patients, the cavity may extend into the medulla oblongata ( syringobulbia) with the development of bilateral lesions of the lower cranial nerves and Horner's syndrome.

Rice. 4. Syringomyelia. MRI of the cervical spinal cord, sagittal projection. Fluid-filled cavity (area of hypointense signal - large arrow) and associated Arnold-Chiari anomaly (small arrow)

Rice. 5... Syringomyelia - clinical manifestations
The pathogenesis of syringomyelia is not well understood; most likely, the development of the disease is associated with impaired CSF hydrodynamics. Many patients have developmental disorders of the brainstem and cerebellum (Arnold-Chiari malformation), in which the cerebellar tonsils are extended and prolapse into the foramen magnum ( cerebellar ectopia). Some patients are shown surgical decompression of the foramen magnum and drainage of the cavity through a syringostomy.
Other common syndromes
Spinal cord syndromes resulting from neurosyphilis (tabes dorsalis) and vitamin B12 deficiency (subacute degeneration of the spinal cord) are common. In spinal cord infarction caused by thrombosis of the anterior spinal artery, the posterior columns usually remain intact.
In patients over 50, the most common cause of myelopathy is spondylosis of the cervical spine... In this case, a degenerative disease (osteoarthritis) of the cervical vertebrae can lead to compression of the spinal cord due to exposure to:
- calcification, degeneration and protrusion of intervertebral discs
- bone growths ( osteophytes)
- calcification and thickening of the longitudinal ligament.
In patients under the age of 40, the most common cause of spinal cord injury is multiple sclerosis. More rare causes are shown in Table 1.
Table 1.
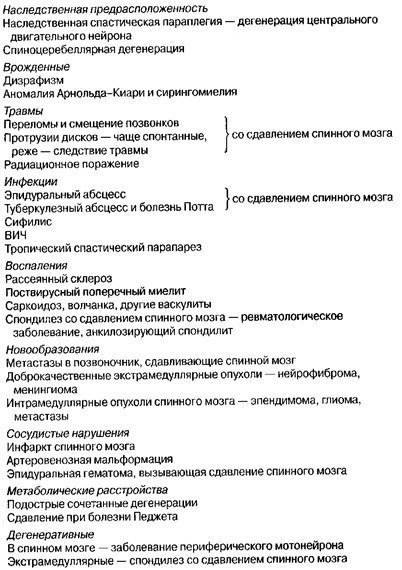
Treatment
When examining a patient with acute myelopathy, the first step is to exclude spinal cord compression — MRI or myelography (Fig. 6). This allows you to identify a disease requiring urgent surgical intervention, or in the case of a malignant neoplasm, determine the indications for radiation therapy and the use of corticosteroids in order to reduce edema. After reducing the severity of spinal cord compression, treatment is carried out aimed at eliminating the cause of the disease (Table 1).

Rice. 6. A sagittal MRI scan showed a meningioma causing compression of the spinal cord. Benign tumors relatively rarely cause compression, but early diagnosis increases the likelihood of successful surgery
Spinal root involvement (radiculopathy)
Clinical neuroanatomy and classification
The nerve roots extend to the left and right of the spinal cord through the intervertebral foramen, where the dorsal (sensory) and ventral (motor) roots join to form the spinal nerves. The spinal nerves are numbered according to the serial number of the vertebrae between which they leave the canal (Fig. 7). In the cervical spine, the number of each root corresponds to the number of the vertebra located below the exit hole. Thus, the C7 root extending between the C6 and C7 vertebrae can be damaged by the protrusion of the C6 / C7 intervertebral disc. However, the nerve between vertebrae C7 and Th10 is numbered C8. The roots in the thoracic, lumbar and sacral regions are numbered in accordance with the serial number of the vertebra above the exit site. Despite this, prolapse of the lumbar intervertebral disc usually injures the root with the same number as the underlying vertebra. For example, prolapse of the L4 / L5 disc damages the L5 nerve, even though L4 exits the opening between L4 / L5. The reason for this is the three-dimensional intraspinal organization of the lumbosacral roots (cauda equina).
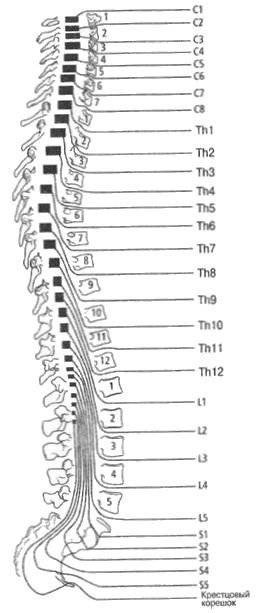
Rice. 7. The interposition of spinal cord segments, vertebral roots
Cervical radiculopathy
Prolapse of the altered intervertebral disc in the cervical spine posteriorly relative to a pair of normally located vertebrae can lead to compression of the nerve at its exit from the opening. Other causes of compression are spondylosis and, much less commonly, tumors.
The clinical manifestations of such a lesion are neck pain radiating along the arm, usually in the innervation zone of the corresponding myotome, less often in the dermatome. Weakness of muscles innervated from the corresponding segment of the spinal cord, loss of tendon reflexes and impaired sensitivity in the corresponding dermatomes are also possible.
In most patients with diseases of the intervertebral discs, as a result of conservative treatment, there is an improvement in their condition. Non-steroidal anti-inflammatory drugs and muscle relaxants are used, individual patients are shown wearing a collar and following the recommendations of a physiotherapist to relieve pain. Few patients are shown MRI to determine the appropriateness of surgery. Surgeries to widen the outlet or remove a herniated disc are more effective in the presence of neurological deficits and functional limitations than solely for relieving pain.
In some cases, protrusion of the intervertebral disc or changes that have arisen as a complication of spondylosis can simultaneously cause compression of the spinal root and the spinal cord itself ( myeloradiculopathy). If compression is observed at the level of closure of tendon reflexes upper limb, a valuable diagnostic criterion for the level of damage is the identification inversion reflexes... For example, if the patient does not have a biceps reflex, percussion on the biceps tendon causes flexion of the finger (inverted biceps reflex), which can be represented as follows:
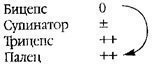
This implies the presence of a lesion at the C5 level, causing an interruption of the reflex arc from the biceps, however, due to the fact that the spinal cord is simultaneously involved in the pathological process, the suprasegmental inhibition of the reflex arc disappears and the flexion reflex of the fingers of the hand appears, the arc of which closes at the level of the C8 segment.
Ponytail
The spinal cord ends with a cone (conus medullaris) at the level of the lower border of the L1 vertebra. The lumbar and sacral roots then follow within the spinal canal before reaching the exit opening and forming the cauda equina. Pathological processes in this area, for example, tumors, usually lead to simultaneous multiple asymmetric root lesions, which is manifested by impaired functions of the peripheral motor neuron and loss of sensitivity. Often, there is also a dysfunction of the bladder, manifested by chronic urinary retention with overflow incontinence and infections of the urethra. Similar symptoms develop when the lower part of the spinal cord itself is damaged ( "Defeat of the cone"), the clinical feature of such a lesion is the simultaneous presence of signs of damage to the central and peripheral motor neurons. Thus, the patient may lack Achilles reflexes in combination with bilateral extensor pathological foot reflexes.
Intermittent cauda equina claudication
Clinical syndrome arising in circulatory disorders of the cauda equina due to narrowing of the lumbar spinal canal in degenerative lesions of the spine. It is characterized by transient neurological symptoms in the form of pain in the buttocks and hips, motor and sensory disorders in the lower extremities, which occur during exertion and disappear at rest, usually in a position with a bent back (in this situation, the lumen of the spinal canal increases). The main direction of differential diagnosis is the elimination of true moving lameness caused by ischemia of the muscles of the legs in case of peripheral circulation failure. This condition differs from spinal lesion in the absence of sensorimotor disorders, as well as in the time of regression of symptoms at rest (1-2 minutes with peripheral vascular insufficiency, 5-15 minutes with intermittent claudication of the cauda equina). Decompression laminectomy leads to an improvement in the condition of stenosis of the lumbar canal, while a preliminary MRI or CT scan is mandatory.
Lumbar disc prolapse
Prolapse of the altered intervertebral disc in the lumbar spine usually leads to compression of the roots, which are directed laterally to the intervertebral foramen, more often the underlying roots are affected. Thus, the S1 root can be compressed by a herniated L5 / S1 disc. Typical manifestations are pain in the lower back, spreading along the back of the leg from the buttock to the ankle ( sciatica), paralysis and weakness of the gastrocnemius and soleus muscles (most clearly noticeable when the patient is standing), loss of sensitivity in the S1 innervation zone, and a decreased Achilles reflex. When the L5 root is damaged, caused by the prolapse of the L4 / L5 disc, the pain spreads along the sciatic nerve and is accompanied by weakness of the foot extensors, in particular, paresis of the lateral extensor longus of the toes and impaired sensitivity in the innervation zone of the L5 dermatome. Passive tension of the lower lumbosacral roots (raising the unbent leg in a supine patient) is limited due to the resulting pain and muscle tension. Pain and muscle tension increase with passive dorsiflexion of the ankle when raised and extended in knee joint leg. A similar sign of damage to the upper lumbar roots is a test for straightening the hip, in which the resulting pain and muscle tension limit the passive extension of the hip in a patient who is in a flexion or semi-flexion position.
Treatment of a patient with sciatica at the initial stage is conservative and implies bed rest with subsequent gradual mobilization. The introduction of anesthetics and corticosteroids into the area of the root passage (under CT guidance) can also improve the condition. Persistent neurological symptoms of root compression can be an indication for surgical intervention, for example, decompression laminecumia and discotomy; preliminary determination of the lesion level on the basis of MRI or CT data is mandatory (Fig. 8).

Rice. eight. Prolapse of the intervertebral disc of the lumbar spine. CT shows lateral disc protrusion (arrow). The patient suffers from sciatica due to root compression
Acute central disc prolapse
In this case, urgent neurosurgical assistance is required. The disc prolapses in the central region, causing total compression of the cauda equina, less often compression of individual roots is observed. Patients experience severe acute back pain, sometimes radiating down the legs, in combination with bilateral weakness of the muscles of the lower extremities (with the absence of Achilles reflexes) and acute painless urinary retention (an increase in the bladder is detected on palpation). Development of persistent constipation or fecal incontinence is possible. The loss of sensation may be limited to the lower sacral dermatomes (saddle anesthesia). The tone of the anal sphincter is reduced, anal reflexes are absent (due to the defeat of the roots S3 - S4 - S5). This reflex is caused by streak irritation of the skin near the anus and normally leads to a contraction of the sphincter. After the diagnosis is confirmed by neuroimaging, an urgent decompression laminectomy is required to prevent irreversible sphincter dysfunction.
Neurology for general practitioners. L. Ginsberg
