1. Functions and development cordially- vascular system
2. The structure of the heart
3. The structure of the arteries
4. The structure of the veins
5. Microcirculatory bed
6. Lymphatic vessels
1. Cardiovascular system formed by the heart, blood and lymph vessels.
Functions of the cardiovascular system:
· Transport - ensuring the circulation of blood and lymph in the body, transporting them to and from organs. This fundamental function consists of trophic (delivery of nutrients to organs, tissues and cells), respiratory (transport of oxygen and carbon dioxide) and excretory (transport of end products of metabolism to the excretory organs) functions;
· Integrative function - the unification of organs and organ systems into a single organism;
· Regulatory function, along with the nervous, endocrine and immune systems, the cardiovascular system is one of the regulatory systems of the body. It is able to regulate the functions of organs, tissues and cells by delivering mediators, biologically active substances, hormones and others to them, as well as by changing the blood supply;
· The cardiovascular system is involved in immune, inflammatory and other general pathological processes (metastasis of malignant tumors and others).
Development of the cardiovascular system
Vessels develop from the mesenchyme. Distinguish between primary and secondary angiogenesis... Primary angiogenesis, or vasculogenesis, is the process of direct, initial formation of the vascular wall from the mesenchyme. Secondary angiogenesis is the formation of blood vessels by their regrowth from existing vascular structures.
Primary angiogenesis
Blood vessels form in the wall of the yolk sac on
The 3rd week of embryogenesis under the inductive influence of the endoderm that is part of it. First, islets of blood are formed from the mesenchyme. Islet cells differentiate into two directions:
· Hematogenous line gives rise to blood cells;
· The angiogenic lineage gives rise to primary endothelial cells, which connect to each other and form the walls of blood vessels.
In the body of the embryo, blood vessels develop later (in the second half of the third week) from the mesenchyme, the cells of which turn into endothelial cells. At the end of the third week, the primary blood vessels of the yolk sac are connected to the blood vessels of the body of the embryo. After the start of blood circulation through the vessels, their structure becomes more complicated, in addition to the endothelium, membranes are formed in the wall, consisting of muscle and connective tissue elements.
Secondary angiogenesis represents the growth of new vessels from those already formed. It is divided into embryonic and postembryonic. After the endothelium is formed as a result of primary angiogenesis, the further formation of vessels occurs only due to secondary angiogenesis, that is, by regrowth from already existing vessels.
Features of the structure and functioning of different vessels depends on the hemodynamic conditions in a given area of the human body, for example: the level of blood pressure, blood flow velocity, and so on.
The heart develops from two sources: the endocardium is formed from the mesenchyme and at first has the form of two vessels - mesenchymal tubes, which later merge to form the endocardium. The myocardium and mesothelium of the epicardium develop from the myoepicardial plate - part of the visceral sheet of the splanchnotome. The cells of this plate differentiate in two directions: myocardial rudiment and epicardial mesothelium rudiment. The rudiment takes an internal position, its cells turn into cardiomyoblasts capable of division. In the future, they gradually differentiate into three types of cardiomyocytes: contractile, conducting and secretory. The mesothelium of the epicardium develops from the rudiment of the mesothelium (mesothelium). Loose fibrous unformed connective tissue of the epicardial lamina propria is formed from the mesenchyme. Two parts - the mesodermal (myocardium and epicardium) and the mesenchymal (endocardium) join together to form the heart, which consists of three membranes.
2. Heart - it is a kind of pump of rhythmic action. The heart is the central organ of the blood and lymph circulation. In its structure, there are features of both a layered organ (has three membranes) and a parenchymal organ: the stroma and parenchyma can be distinguished in the myocardium.
Heart functions:
· Pumping function - constantly decreasing, maintains a constant level of blood pressure;
Endocrine function - the production of natriuretic factor;
· Information function - the heart encodes information in the form of parameters of blood pressure, blood flow velocity and transmits it to tissues, changing metabolism.
The endocardium consists from four layers: endothelial, subendothelial, muscular-elastic, external connective tissue. Epithelial the layer lies on the basement membrane and is represented by a single-layer squamous epithelium. Subendothelial the layer is formed by loose fibrous loose connective tissue. These two layers are analogous to the inner lining of a blood vessel. Muscular-elastic the layer is formed by smooth myocytes and a network of elastic fibers, an analogue of the middle membrane of blood vessels ... External connective tissue the layer is formed by loose fibrous unformed connective tissue and is analogous to the outer shell of the vessel. It connects the endocardium to the myocardium and continues into its stroma.
Endocardium forms duplicates - heart valves - dense plates of fibrous connective tissue with a small content of cells, covered with endothelium. The atrial side of the valve is smooth, while the ventricular side is uneven, has outgrowths to which tendon filaments are attached. The blood vessels in the endocardium are located only in the outer connective tissue layer, therefore, its nutrition is carried out mainly by the diffusion of substances from the blood, which is located both in the heart cavity and in the vessels of the outer layer.
Myocardium is the most powerful shell of the heart, it is formed by cardiac muscle tissue, the elements of which are cardiomyocyte cells. The set of cardiomyocytes can be considered as myocardial parenchyma. The stroma is represented by interlayers of loose fibrous loose connective tissue, which are normally poorly expressed.
Cardiomyocytes are divided into three types:
· The bulk of the myocardium is made up of working cardiomyocytes, they have a rectangular shape and are connected to each other with the help of special contacts - insertion disks. Due to this, they form a functional synthesia;
· Conducting or atypical cardiomyocytes form the conducting system of the heart, which provides a rhythmic coordinated contraction of its various parts. These cells are genetically and structurally muscular, functionally resemble nerve tissue, as they are capable of forming and rapidly conducting electrical impulses.
There are three types of conducting cardiomyocytes:
· P-cells (pacemaker cells) form a sinoauricular node. They differ from working cardiomyocytes in that they are capable of spontaneous depolarization and the formation of an electrical impulse. The wave of depolarization is transmitted through the nexuses to typical atrial cardiomyocytes, which contract. In addition, excitation is transmitted to intermediate atypical cardiomyocytes of the atrioventricular node. Generation of impulses by P-cells occurs at a frequency of 60-80 per minute;
· Intermediate (transitional) cardiomyocytes of the atrioventricular node transmit excitation to working cardiomyocytes, as well as to the third type of atypical cardiomyocytes - Purkinje fiber cells. Transient cardiomyocytes are also capable of independently generating electrical impulses, but their frequency is lower than the frequency of impulses generated by pacemaker cells, and leaves 30-40 per minute;
· Fiber cells - the third type of atypical cardiomyocytes, of which the His bundle and Purkinje fibers are built. The main function of fiber cells is the transmission of excitation from intermediate atypical cardiomyocytes to working ventricular cardiomyocytes. In addition, these cells are capable of independently generating electrical impulses with a frequency of 20 or less per minute;
· Secretory cardiomyocytes are located in the atria, the main function of these cells is the synthesis of natriuretic hormone. It is released into the blood when a large amount of blood enters the atrium, that is, when there is a threat of increased blood pressure. Released into the bloodstream, this hormone acts on the kidney tubules, preventing the reverse reabsorption of sodium into the blood from the primary urine. At the same time, water is released from the body in the kidneys along with sodium, which leads to a decrease in the volume of circulating blood and a drop in blood pressure.
Epicard- the outer shell of the heart, it is the visceral layer of the pericardium - the heart bag. The epicardium consists of two sheets: the inner layer, represented by loose fibrous loose connective tissue, and the outer layer, a single-layer squamous epithelium (mesothelium).
Blood supply to the heart carried out by the coronary arteries originating from the aortic arch. Coronary arteries have a highly developed elastic frame with pronounced external and internal elastic membranes. The coronary arteries branch strongly to capillaries in all membranes, as well as in the papillary muscles and tendon cords of the valves. Vessels are also contained at the base of the heart valves. From the capillaries, blood is collected in the coronary veins, which pour blood either into the right atrium or into the venous sinus. An even more intensive blood supply has a conductive system, where the density of capillaries per unit area is higher than in the myocardium.
Features of lymphatic drainage of the heart is that in the epicardium the lymphatic vessels accompany the blood vessels, while in the endocardium and myocardium they form their own abundant networks. Lymph from the heart flows into the lymph nodes in the area of the aortic arch and the lower trachea.
The heart receives both sympathetic and parasympathetic innervation.
Stimulation of the sympathetic part of the autonomic nervous system causes an increase in strength, heart rate and the rate of conduction of excitation through the heart muscle, as well as expansion of the coronary vessels and an increase in the blood supply to the heart. Stimulation of the parasympathetic nervous system causes effects opposite to those of the sympathetic nervous system: a decrease in the frequency and strength of heart contractions, myocardial excitability, narrowing of the coronary vessels with a decrease in the blood supply to the heart.
3. Blood vessels are organs of the layered type. They consist of three membranes: inner, middle (muscular) and outer (adventitious). Blood vessels are divided into:
· Arteries that carry blood from the heart;
• veins through which blood moves to the heart;
· Vessels of the microvasculature.
The structure of blood vessels depends on hemodynamic conditions. Hemodynamic conditions- these are the conditions for the movement of blood through the vessels. They are determined by the following factors: the value of blood pressure, blood flow velocity, blood viscosity, the effect of the Earth's gravitational field, the location of the vessel in the body. Hemodynamic conditions determine such morphological signs of blood vessels as:
· Wall thickness (in the arteries it is more, and in the capillaries - less, which facilitates the diffusion of substances);
· The degree of development of the muscular membrane and the direction of smooth myocytes in it;
· The ratio in the middle shell of the muscle and elastic components;
· Presence or absence of inner and outer elastic membranes;
· The depth of the vessels;
· Presence or absence of valves;
· The ratio between the thickness of the vessel wall and the diameter of its lumen;
· The presence or absence of smooth muscle tissue in the inner and outer shells.
By the diameter of the artery are divided into arteries of small, medium and large caliber. According to the quantitative ratio in the middle shell of the muscular and elastic components, they are subdivided into elastic, muscular and mixed arteries.
Elastic type arteries
These vessels include the aorta and pulmonary arteries; they perform the transport function and the function of maintaining pressure in the arterial system during diastole. In this type of vessels, the elastic frame is highly developed, which allows the vessels to stretch strongly, while maintaining the integrity of the vessel.
Elastic type arteries are built according to the general principle of the structure of blood vessels and consist of an inner, middle and outer shell. Inner shell rather thick and formed by three layers: endothelial, podendothelial and elastic fiber layer. In the endothelial layer, the cells are large, polygonal; they lie on the basement membrane. The podendothelial layer is formed by loose fibrous loose connective tissue, which contains many collagen and elastic fibers. The inner elastic membrane is missing. Instead, on the border with the middle shell is a plexus of elastic fibers, consisting of an inner circular and outer longitudinal layers. The outer layer passes into the plexus of elastic fibers of the middle shell.
Middle shell consists mainly of elastic elements. In an adult, they form 50-70 fenestrated membranes, which lie at a distance of 6-18 microns from each other and each have a thickness of 2.5 microns. Loose fibrous unformed connective tissue with fibroblasts, collagen, elastic and reticular fibers, smooth myocytes is located between the membranes. In the outer layers of the middle shell are the vessels of the vessels that feed the vascular wall.
Outer adventitia relatively thin, consists of loose fibrous loose connective tissue, contains thick elastic fibers and bundles of collagen fibers running longitudinally or obliquely, as well as vascular vessels and vascular nerves formed by myelin and myelin-free nerve fibers.
Arteries of mixed (muscular-elastic) type
An example of a mixed type artery is the axillary and carotid arteries. Since the pulse wave gradually decreases in these arteries, along with the elastic component, they have a well-developed muscle component to maintain this wave. The wall thickness in these arteries increases significantly in comparison with the diameter of the lumen.
Inner shell represented by endothelial, subendothelial layers and an internal elastic membrane. In the middle shell both muscular and elastic components are well developed. Elastic elements are represented by individual fibers that form a network, fenestrated membranes and layers of smooth myocytes lying between them, running in a spiral. Outer sheath formed by loose fibrous loose connective tissue, in which bundles of smooth myocytes are found, and an external elastic membrane lying immediately behind the middle membrane. The outer elastic membrane is somewhat less pronounced than the inner one.
Muscular arteries
These arteries include arteries of small and medium caliber lying near organs and intraorgan. In these vessels, the strength of the pulse wave is significantly reduced, and it becomes necessary to create additional conditions for the advancement of blood, therefore, the muscle component predominates in the middle shell. The diameter of these arteries can decrease due to contraction and increase due to relaxation of smooth myocytes. The wall thickness of these arteries significantly exceeds the diameter of the lumen. Such vessels create resistance to the driving blood, which is why they are often called resistive.
Inner shell has a small thickness and consists of endothelial, podendothelial layers and an internal elastic membrane. Their structure is generally the same as in mixed type arteries, and the inner elastic membrane consists of one layer of elastic cells. The middle shell consists of smooth myocytes arranged in a gentle spiral, and a loose network of elastic fibers, also spiraling. The spiral arrangement of myocytes contributes to a greater decrease in the lumen of the vessel. The elastic fibers merge with the outer and inner elastic membranes to form a single frame. Outer sheath formed by an external elastic membrane and a layer of loose fibrous loose connective tissue. It contains blood vessels of blood vessels, sympathetic and parasympathetic nerve plexuses.
4. The structure of the veins, as well as arteries, depends on hemodynamic conditions. In the veins, these conditions depend on whether they are located in the upper or lower body, since the structure of the veins of these two zones is different. There are veins of the muscular and non-muscular types. To the veins of the muscleless type include the veins of the placenta, bones, pia mater, retina, nail bed, trabeculae of the spleen, central veins of the liver. The absence of a muscular membrane in them is explained by the fact that the blood here moves under the influence of gravity, and its movement is not regulated by muscle elements. These veins are built from the inner membrane with the endothelium and podendothelial layer and the outer membrane of loose fibrous loose connective tissue. The inner and outer elastic membranes, as well as the middle shell, are absent.
Veins of the muscle type are subdivided into:
· Veins with poor development of muscle elements, these include small, medium and large veins of the upper body. Veins of small and medium caliber with poor muscular development are often located intraorgan. The podendothelial layer in small and medium-sized veins is relatively poorly developed. Their muscular membrane contains a small number of smooth myocytes, which can form separate clusters that are distant from each other. The sections of the vein between such clusters are able to expand sharply, performing a depositing function. The middle shell is represented by a small amount of muscle elements, the outer shell is formed by loose fibrous loose connective tissue;
Veins with medium development of muscle elements, an example of this type of vein is the brachial vein. The inner membrane consists of the endothelial and subendothelial layers and forms duplicate valves with a large number of elastic fibers and smooth myocytes located longitudinally. The inner elastic membrane is absent; it is replaced by a network of elastic fibers. The middle shell is formed by spirally lying smooth myocytes and elastic fibers. The outer membrane is 2-3 times thicker than that of the artery, and it consists of longitudinally lying elastic fibers, individual smooth myocytes and other components of loose fibrous unformed connective tissue;
Veins with a strong development of muscle elements, an example of this type of veins are the veins of the lower body - the inferior vena cava, the femoral vein. These veins are characterized by the development of muscle elements in all three membranes.
5. Microcirculatory bed includes the following components: arterioles, precapillaries, capillaries, postcapillaries, venules, arterio-venular anastomoses.
The functions of the microvasculature are as follows:
Trophic and respiratory functions, since the exchange surface of capillaries and venules is 1000 m2, or 1.5 m2 per 100 g of tissue;
· Depositing function, since a significant part of the blood is deposited in the vessels of the microvasculature at rest, which is included in the bloodstream during physical work;
· Drainage function, since the microvasculature collects blood from the bringing arteries and distributes it throughout the organ;
· Regulation of blood flow in the organ, this function is performed by arterioles due to the presence of sphincters in them;
· Transport function, that is, blood transport.
Three links are distinguished in the microvasculature: arterial (arterioles precapillaries), capillary and venous (postcapillaries, collecting and muscle venules).
Arterioles have a diameter of 50-100 microns. In their structure, three membranes are preserved, but they are less pronounced than in the arteries. In the area where the capillary arteriole leaves, there is a smooth muscle sphincter that regulates blood flow. This area is called the precapillary.
Capillaries- these are the smallest vessels, they vary in size on the:
· Narrow type 4-7 microns;
· Normal or somatic type 7-11 microns;
· Sinusoidal type 20-30 microns;
· Lacunar type 50-70 microns.
A layered principle is traced in their structure. The inner layer is formed by the endothelium. The endothelial layer of the capillary is an analogue of the inner shell. It lies on the basement membrane, which first splits into two sheets and then joins. As a result, a cavity is formed in which pericyte cells lie. On these cells, these cells end with autonomic nerve endings, under the regulatory action of which the cells can accumulate water, increase in size and close the lumen of the capillary. When water is removed from the cells, they decrease in size, and the lumen of the capillaries opens. Functions of pericytes:
· Change in the lumen of the capillaries;
· Source of smooth muscle cells;
· Control of proliferation of endothelial cells during capillary regeneration;
· Synthesis of components of the basement membrane;
· Phagocytic function.
Basement membrane with pericytes- analogue of the middle shell. Outside of it is a thin layer of the basic substance with adventitia cells, which play the role of a cambium for loose fibrous unformed connective tissue.
Organ specificity is characteristic of capillaries, and therefore three types of capillaries:
· Capillaries of the somatic type or continuous, they are located in the skin, muscles, brain, spinal cord. They are characterized by a continuous endothelium and a continuous basement membrane;
Capillaries of fenestrated or visceral type (localization - internal organs and endocrine glands). They are characterized by the presence of constrictions in the endothelium - fenestra and a continuous basement membrane;
Intermittent or sinusoidal capillaries (red Bone marrow, spleen, liver). In the endothelium of these capillaries there are true openings, they are also in the basement membrane, which may be absent altogether. Sometimes capillaries include lacunas - large vessels with a wall structure like in a capillary (cavernous bodies of the penis).
Venules are divided into postcapillary, collective and muscular. Postcapillary venules are formed as a result of the fusion of several capillaries, have the same structure as a capillary, but a larger diameter (12-30 microns) and a large number of pericytes. In the collecting venules (diameter 30-50 microns), which are formed when several postcapillary venules merge, there are already two pronounced membranes: the inner one (endothelial and subendothelial layers) and the outer one - loose fibrous unformed connective tissue. Smooth myocytes appear only in large venules reaching a diameter of 50 μm. These venules are called muscle venules and are up to 100 microns in diameter. Smooth myocytes in them, however, do not have a strict orientation and form a single layer.
Arterio-venular anastomoses or shunts- this is a type of vessels in the microcirculatory bed, through which blood from arterioles enters the venules, bypassing the capillaries. This is necessary, for example, in the skin for thermoregulation. All arterio-venular anastomoses are divided into two types:
• true - simple and complex;
· Atypical anastomoses or shunts.
In simple anastomoses there are no contractile elements, and the blood flow in them is regulated by the sphincter located in the arterioles at the site of the anastomosis. In complex anastomoses there are elements in the wall that regulate their lumen and the intensity of blood flow through the anastomosis. Complex anastomoses are divided into glomus-type anastomoses and trailing artery-type anastomoses. In anastomoses of the type of guard arteries in the inner membrane there are accumulations of longitudinally smooth myocytes. Their contraction leads to protrusion of the wall in the form of a pillow into the lumen of the anastomosis and its closure. In anastomoses such as a glomerulus (glomerulus), there is an accumulation of epithelioid E-cells (in the form of an epithelium) in the wall, capable of sucking in water, increasing in size and closing the lumen of the anastomosis. With the release of water, the cells decrease in size, and the lumen opens. There are no contractile elements in the half-shunts in the wall, the width of their lumen is not regulated. Venous blood from venules can be thrown into them, therefore mixed blood flows in half shunts, in contrast to shunts. Anastomoses perform the function of blood redistribution, blood pressure regulation.
6. Lymphatic system conducts lymph from tissues to the venous bed. It consists of lymphocapillaries and lymphatic vessels. Lymphocapillaries start blindly in tissues. Their wall often consists only of the endothelium. The basement membrane is usually absent or poorly expressed. To prevent the capillary from collapsing, there are sling or anchor filaments, which are attached to the endotheliocytes at one end, and are woven into the loose fibrous connective tissue at the other. The diameter of the lymphocapillaries is 20-30 microns. They perform a drainage function: they suck in tissue fluid from the connective tissue.
Lymphatic vessels divided into intraorganic and extraorganic, as well as the main (chest and right lymphatic ducts). By diameter, they are divided into small, medium and large lymphatic vessels. In vessels of small diameter, there is no muscular sheath, and the wall consists of an inner and an outer shell. The inner shell consists of the endothelial and subendothelial layers. The subendothelial layer is gradual, without sharp boundaries. It passes into a loose fibrous unformed connective tissue of the outer shell. Vessels of medium and large caliber have a muscular membrane and are similar in structure to veins. The large lymphatic vessels have elastic membranes. The inner shell forms the valves. In the course of the lymphatic vessels, there are lymph nodes, the passages through which, the lymph is cleansed and enriched with lymphocytes.
Heart(cor) is a hollow four-chambered muscular organ that pumps oxygen-enriched blood into the artery and receives venous blood.
The heart consists of two atria that receive blood from the veins and push it into the ventricles (right and left). The right ventricle supplies blood to the pulmonary arteries through the pulmonary trunk, while the left ventricle supplies blood to the aorta. The left half of the heart contains arterial blood, and the right half of the heart contains venous blood, the right and left halves of the heart are not normally communicated.
The heart is distinguished: three surfaces - pulmonary (facies pulmonalis), sternocostal (facies sternocostalis) and diaphragmatic (facies diaphragmatica); the top (apex cordis) and the base (basis cordis). The border between the atria and the ventricles is the coronary sulcus (sulcus coronarius).
Right atrium(atrium dextrum) is separated from the left by the atrial septum (septum interatriale) and has an additional cavity - the right ear (auricula dextra). There is a depression in the septum - an oval fossa surrounded by the edge of the same name, formed after the oval opening is overgrown.
The right atrium has openings of the superior vena cava (ostium venae cavae superioris) and the inferior vena cava (ostium venae cavae inferioris), delimited by the intervenous tubercle (tuberculum intervenosum) and the opening of the coronary sinus (ostium sinus coronarii). On the inner wall of the right ear there are comb muscles (mm pectinati), ending with a border ridge separating the venous sinus from the cavity of the right atrium.
The right atrium communicates with the ventricle through the right atrioventricular opening (ostium atrioventriculare dextrum).
Right ventricle(ventriculus dexter) is separated from the left interventricular septum (septum interventriculare), in which the muscular and membranous parts are distinguished; has an opening of the pulmonary trunk in front (ostium trunci pulmonalis) and behind - the right atrioventricular opening (ostium atrioventriculare dextrum). The latter is covered with a tricuspid valve (valva tricuspidalis), which has anterior, posterior and septal valves. The leaflets are held in place by tendinous chords, due to which the leaflets are not everted into the atrium.
On the inner surface of the ventricle there are fleshy trabeculae (trabeculae carneae) and papillary muscles (mm. Papillares), from which tendon chords begin. The opening of the pulmonary trunk is covered with a valve of the same name, consisting of three semilunar valves: front, right and left (valvulae semilunares anterior, dextra et sinistra).
Left atrium(atrium sinistrum) has a cone-shaped extension facing anteriorly - the left ear (auricular sinistra) - and five openings: four openings of the pulmonary veins (ostia venarum pulmonalium) and the left atrioventricular opening (ostium atrioventriculare sinistrum).
Left ventricle(ventriculus sinister) has a left atrioventricular opening behind, covered by a mitral valve (valva mitralis), consisting of anterior and posterior cusps, and aortic openings, covered by a valve of the same name, consisting of three semilunar valves: posterior, right and left (valvulae semilunares posterior , dextra et sinistra). There are sinuses between the flaps and the aortic wall. On the inner surface of the ventricle there are fleshy trabeculae (trabeculae carneae), anterior and posterior papillary muscles (mm.papillares anterior et posterior).
2. STRUCTURE OF THE HEART WALL. HEART CONDUCTIVE SYSTEM. STRUCTURE OF THE PERICARDIUM
Wall of the heart consists of a thin inner layer - the endocardium (endocardium), the middle developed layer - the myocardium (myocardium) and the outer layer - the epicardium (epicardium).
The endocardium lines the entire inner surface of the heart with all its formations.
The myocardium is formed by the cardiac striated muscle tissue and consists of cardiac cardiomyocytes, which provides a complete and rhythmic contraction of all chambers of the heart. The muscle fibers of the atria and ventricles start from the right and left (anuli fibrosi dexter et sinister) fibrous rings, which are part of the soft skeleton of the heart. The annulus fibrosus surround the corresponding atrioventricular openings, providing support for their valves.
The myocardium consists of three layers. The outer oblique layer at the apex of the heart passes into the curl of the heart (vortex cordis) and continues into the deep layer. The middle layer is formed by circular fibers. The epicardium is built on the principle of the serous membranes and is the visceral layer of the serous pericardium. The epicardium covers the outer surface of the heart from all sides and the initial sections of the vessels departing from it, passing along them into the parietal plate of the serous pericardium.
The normal contractile function of the heart is provided by conducting system, the centers of which are:
1) sinus-atrial node (nodus sinuatrialis), or Kis-Fleck's node;
2) the atrioventricular node (nodus atrioventricularis), or the Fschoff-Tavara node, passing downward into the atrioventricular bundle (fasciculus atrioventricularis), or the bundle of His, which is divided into the right and left legs (cr dextrum et sinistrum).
Pericardium (pericardium) is a fibro-serous sac in which the heart is located. The pericardium is formed by two layers: the outer (fibrous pericardium) and the inner (serous pericardium). The fibrous pericardium passes into the adventitia of the large vessels of the heart, and the serous one has two plates - parietal and visceral, which pass into each other in the region of the base of the heart. Between the plates there is a pericardial cavity (cavitas pericardialis), it contains a small amount of serous fluid. In the pericardium, three sections are distinguished: the anterior, or sternocostal, right and left mediastinal sections, the lower, or diaphragmatic, section.
The blood supply to the pericardium is carried out in the branches of the superior phrenic arteries, branches of the thoracic aorta, branches of the pericardio-diaphragmatic artery.
Venous outflow is carried out in the azygos and semi-unpaired veins.
Lymphatic drainage is carried out into the anterior and posterior mediastinal, pericardial and pre-pericardial lymph nodes.
Innervation: branches of the right and left sympathetic trunks, branches of the phrenic and vagus nerves.
3. BLOOD SUPPLY AND HEART INERVATION
The arteries of the heart originate from the aortic bulb (bulbus aortae).
The right coronary artery (a coronaria dextra) has a large branch - the posterior interventricular branch (ramus interventricularis posterior).
The left coronary artery (a.coronaria sinistra) is divided into the envelope (r. Circumflexus) n anterior interventricular branches (r. Interventricularis anterior). These arteries combine to form transverse and longitudinal arterial rings.
Small (v. Cordis parva), middle (v. Cordis media) and large veins of the heart (v. Cordis magna), oblique (v. Oblique atrii sinistri) and posterior veins of the left ventricle (v. Posterior ventriculi sinistri) form the coronary sinus ( sinus coronarius). In addition to these veins, there are the smallest (vv. Cordis minimae) and anterior veins of the heart (vv. Cordis anteriores).
Lymphatic drainage is carried out into the anterior mediastinal and one of the lower tracheobronchial lymph nodes.
Innervation:
1) cardiac nerves originating from the cervical and upper thoracic nodes of the right and left lymphatic trunks;
2) superficial extraorganic cardiac plexus;
3) deep extraorganic cardiac plexus;
4) intraorgan cardiac plexus (formed by the branches of extraorgan cardiac plexuses).
4. PULMONARY TRUNK AND ITS BRANCHES. STRUCTURE OF THE AORTA AND ITS BRANCHES
Pulmonary trunk(truncus pulmonalis) is divided into right and left pulmonary arteries. The place of division is called the bifurcation of the pulmonary trunk (bifurcatio trunci pulmonalis).
Right pulmonary artery(a. pulmonalis dextra) enters the gate of the lung and divides. In the upper lobe, the descending and ascending posterior branches (rr. Posteriores descendens et ascendens), the apical branch (r. Apicalis), the descending and ascending front branches (rr. Anteriores descendens et ascendens) are distinguished. In the middle lobe, medial and lateral branches are distinguished (rr.lobi medii medialis et lateralis). In the lower lobe - the upper branch of the lower lobe (r. Superior lobi inferioris) and the basal part (pars basalis), which is divided into four branches: anterior and posterior, lateral and medial.
Left pulmonary artery(a. pulmonalis sinistra), entering the gate of the left lung, is divided into two parts. The ascending and descending front (rr. Anteriores ascendens et descendens), reed (r. Lingularis), back (r. Posterior) and apical branches (r. Apicalis) go to the upper lobe. The upper branch of the lower lobe goes to the lower lobe of the left lung, the basal part is divided into four branches: anterior and posterior, lateral and medial (as in the right lung).
Pulmonary veins originate from the capillaries of the lung.
The right lower pulmonary vein (v. Pulmonalis dextra inferior) collects blood from five segments of the lower lobe of the right lung. This vein forms when the superior vein of the inferior lobe and the common basal vein merge.
The right upper pulmonary vein (v. Pulmonalis dextra superior) collects blood from the upper and middle lobes of the right lung.
The left lower pulmonary vein (v. Pulmonalis sinistra inferior) collects blood from the lower lobe of the left lung.
The left upper pulmonary vein (v. Pulmonalis sinistra superior) collects blood from the upper lobe of the left lung.
The right and left pulmonary veins flow into the left atrium.
Aorta(aorta) has three sections: the ascending part, the arch and the descending part.
Ascending part of the aorta(pars ascendens aortae) has an extension in the initial section - the aortic bulb (bulbus aortae), and at the location of the valve - three sinuses.
Aortic arch(arcus aortae) originates at the level of the articulation of the II right costal cartilage with the sternum; has a slight narrowing, or isthmus of the aorta (isthmus aortae).
Descending part of the aorta(pars descendens aortae) begins at level IV of the thoracic vertebra and continues to IV lumbar vertebra where it divides into the right and left common iliac arteries. In the descending part, the chest (pars thoracica aortae) and abdominal parts (pars abdominalis aortae) are isolated.
5. SHOULDER SHAFT. EXTERNAL CAROTID ARTERY
Brachiocephalic trunk(truncus brachiocephalicus) is located in front of the trachea and behind the right brachiocephalic vein, departing from the aortic arch at level II of the right costal cartilage; at the level of the right sternoclavicular joint, it is divided into the right common carotid and right subclavian arteries, which are its terminal branches. The left common carotid artery (a. Carotis communis sinistra) departs from the aortic arch itself.
External carotid artery(a. carotis externa) is one of the two branches of the common carotid artery, which gives off many branches.
Anterior branches of the external carotid artery .
Superior thyroid artery(a. thyroidea superior) at the upper pole of the thyroid lobe is divided into anterior and posterior branches. This artery has lateral branches:
1) subhyoid branch (r. Infrahyoideus);
2) sternocleidomastoid branch (r. Sternocleidomastoidea);
3) the superior laryngeal artery (a. Laryngea superior);
4) cricothyroid branch (r. Cricothyroideus).
(Lingual artery(a. lingualis) departs at the level of the large horn of the hyoid bone, gives off dorsal branches, and its final branch is the deep artery of the tongue (a. profunda linguae); before entering the language, it gives two more branches: the sublingual artery (a. sublingualis) and the suprahyoid branch (rü suprahyoideus).
Facial artery(ayu facialis) originates just above the lingual artery. The face gives the following branches:
1) the upper labial artery (a. Labialis inferior);
2) lower labial artery (a. Labialis superior);
3) angular artery (a. Angularis).
On the neck, the facial artery gives the following branches:
1) amygdala branch (r. Tonsillaris);
2) chin artery (a. Submentalis);
3) the ascending palatine artery (a. Palatine ascendens).
((bi) Posterior branches of the external carotid artery .
The posterior ear artery (a.auricularis posterior) gives the following branches:
1) the occipital branch (r. Occipitalis);
2) the ear branch (r. Auricularis);
3) the styloid artery (a. Stylomastoidea), giving the posterior tympanic artery (a. Tympanica posterior).
The occipital artery (a.occipitalis) gives the following branches:
1) auricular branch (r. Auricularis);
2) descending branch (r. Descendens);
3) sternocleidomastoid branches (rr.sternocleidomastoidea);
4) mastoid branch (r. Mastoideus).
The ascending pharyngeal artery (a.pharyngea ascendens) gives the following branches:
1) pharyngeal branches (rr. Pharyngealis);
2) the lower tympanic artery (a.tympanica inferior);
3) posterior meningeal artery (a. Meningea posterior).
Terminal branches of the external carotid artery.
Maxillary artery(a. maxillaries), in which there are three sections - jaw, pterygoid, pterygo-palatine, from which their branches branch off.
Branches of the jaw:
1) anterior tympanic artery (a.tympanica anterior);
2) deep ear artery (a. Auricularis profunda);
3) the middle meningeal artery (a. Meningea media), giving the superior tympanic artery (a. Tympanica superior), frontal and parietal branches (rr. Frontalis et parietalis);
4) lower alveolar artery (a.alveolaris inferior).
Pterygoid branches:
1) pterygoid branches (rr. Pterigoidei);
2) the chewing artery (a. Masseterica);
3) buccal artery (a. Buccalis);
4) anterior and posterior temporal arteries (rr. Temporales anterioris et posterioris);
5) the posterior superior alveolar artery (a.alveolaris superior posterior).
Branches of the pterygo-palatine department:
1) the descending palatine artery (a. Palatine descendens);
2) the wedge-palatine artery (a. Sphenopalatina), giving the posterior septal branches (rr. Septales posteriores) and lateral posterior nasal arteries (aa. Nasales posteriores laterales);
3) infraorbital artery (a. Infraorbitalis), giving the anterior superior alveolar arteries (aa. Alveolares superiores anteriores).
6. BRANCHES OF THE INTERNAL CAROTID ARTERY
Internal carotid artery(a. carotis interna) carries out the blood supply to the brain and organs of vision. The following parts are distinguished in it: cervical (pars cervicalis), stony (pars petrosa), cavernous (pars cavernosa) and cerebral (pars cerebralis). The cerebral part of the artery gives off the ophthalmic artery and divides into its terminal branches (anterior and middle cerebral arteries) at the inner edge of the anterior inclined process.
Branches of the ophthalmic artery(a. ophthalmica):
1) the central retinal artery (a. Centralis retinae);
2) the lacrimal artery (a. Lacrimalis);
3) posterior ethmoidal artery (a. Ethmoidalis posterior);
4) anterior ethmoidal artery (a. Ethmoidalis anterior);
5) long and short posterior ciliary arteries (aa. Ciliares posteriores longae et breves);
6) anterior ciliary arteries (aa. Ciliares anteriores);
7) muscle arteries (aa. Musculares);
8) the medial arteries of the eyelids (aa. Palpebrales mediales); anastomose with the lateral arteries of the eyelids, form the arch of the upper eyelid and the arch of the lower eyelid;
9) supra-block artery (a. Supratrochlearis);
10) dorsal artery of the nose (a. Dorsalis nasi).
V middle cerebral artery(a. cerebri media) distinguish between wedge-shaped (pars sphenoidalis) and insular parts (pars insularis), the latter continues into the cortical part (pars corticalis).
Anterior cerebral artery(a. cerebri anterior) connects to the opposite side of the artery of the same name by means of the anterior communicating artery (a. communicans anterior).
Posterior communicating artery(a. communicans posterior) is one of the anastomoses between the branches of the internal and external carotid arteries.
Anterior villous artery(a choroidea anterior).
7. BRANCHES OF THE CONNECTIVE ARTERY
In this artery, three sections are distinguished: the vertebral, internal thoracic arteries and the thyroid trunk depart from the first, the costal-cervical trunk from the second, and the non-permanent transverse neck artery from the third.
Branches of the first section:
1) vertebral artery(a. vertebralis), in which four parts are distinguished: prevertebral (pars prevertebralis), cervical (pars cervicalis), atlantic (pars atlantica) and intracranial (pars intracranialis).
Branches of the cervical part:
a) radicular branches (rr. radiculares);
b) muscle branches (rr. musculares).
Intracranial branches:
a) anterior spinal artery (a.spinalis anterior);
b) posterior spinal artery (a. spinalis posterior);
c) meningeal branches (rr. meningei) - front and back;
d) posterior lower cerebellar artery (a. inferior posterior cerebri).
The basilar artery (a.basilaris) is located in the groove of the bridge of the same name and gives the following branches:
a) labyrinth artery (a. labyrinthi);
b) middle cerebral arteries (aa. mesencephalicae);
c) the superior cerebellar artery (a. superior cerebelli);
d) anterior lower cerebellar artery (a. inferior anterior cerebelli);
e) bridge arteries (aa. pontis).
The right and left posterior cerebral arteries (aa. Cerebri posterior) close the arterial circle from behind, the posterior communicating artery flows into the posterior cerebral artery, resulting in the formation of the arterial circle of the large brain (circulus arteriosus cerebri);
2) internal mammary artery(a. thoracica interna) gives:
a) bronchial and tracheal branches (rr. bronchiales et tracheales);
b) sternal branches (rr. sternales);
c) mediastinal branches (rr. mediastinales);
d) perforating branches (rr. perforantes);
e) thymic branches (rr. thymici);
f) pericardial diaphragmatic artery (a.pericardiacophrenica);
g) musculophrenic artery (a. musculophrenica);
h) the upper epigastric artery (a.epigastrica superior);
i) anterior intercostal branches (rr. intercostals anteriores);
3) shield-neck trunk(truncus thyrocervicalis) is divided into three branches:
a) lower thyroid artery (a. thyroidea inferior), giving tracheal branches (rr. tracheales), lower laryngeal artery (a. laryngealis inferior), pharyngeal and esophageal branches (rr. pharyngeales et oesophageales);
b) the suprascapular artery (a. suprascapularis), giving the acromial branch (r. acromialis);
c) the transverse neck artery (a. transversa cervicis), which is divided into superficial and deep branches.
Branches of the second section.
Costal-cervical trunk(truncus costocervicalis) is divided into deep cervical artery (a. cervicalis profunda) and the highest intercostal artery (a. intercostalis suprema).
Axillary artery(a. axillaris) is divided into three sections, is a continuation of the axillary artery.
Branches of the first section:
1) the upper thoracic artery (a.thoracica superior);
2) subscapular branches (rr. Subscapulares);
3) thoracoacromial artery (a. Thoracoacromialis); gives four branches: pectoral (rr. pectorales), subclavian (r. clavicularis), acromial (r. acromialis) and deltoid (r. deltoideus).
Branches of the second section:
1) lateral thoracic artery (a.thoracica lateralis). Gives the lateral branches of the mammary gland (rr. Mammarii lateralis).
Branches of the third section:
1) the anterior artery, the envelope of the humerus (a. Circumflexa anterior humeri);
2) the posterior artery, the envelope of the humerus (a. Circumflexa posterior humeri);
3) the subscapular artery (a. Subscapularis), dividing into the artery, the circumflex scapula (a. Circumflexa scapulae), and the thoracic artery (a. Thoracodorsalis).
8. SHOULDER ARTERY. ELBOW ARTERY. BRANCHES OF THE CHEST AORTE
Brachial artery(a. brachialis) is a continuation of the axillary artery, gives the following branches:
1) the upper ulnar collateral artery (a.collateralis ulnaris superior);
2) the lower ulnar collateral artery (a. Collateralis ulnaris inferior);
3) deep artery of the shoulder (a.profunda brachii), giving the following branches: middle collateral artery (a.collateralis media), radial collateral artery (a.collateralis radialis), deltoid branch (r. Deltoidei) and arteries feeding the humerus ( aa.nutriciae humeri).
Radial artery(a. radialis) is one of the two terminal branches of the brachial artery. The terminal section of this artery forms a deep palmar arch (arcus palmaris profundus), anastomosing with the deep palmar branch of the ulnar artery. Branches of the radial artery:
1) superficial palmar branch (r. Palmaris superficialis);
2) radial recurrent artery (a. Reccurens radialis);
3) dorsal carpal branch (r. Carpalis dorsalis); participates in the formation of the dorsal network of the wrist (rete carpale dorsale);
4) palmar carpal branch (r. Carpalis palmaris).
Ulnar artery(a. ulnaris) is the second terminal branch of the brachial artery. The terminal section of this artery forms a superficial palmar arch (arcus palmaris supreficialis), anastomosing with the superficial palmar branch of the radial artery. Branches of the ulnar artery:
2) muscle branches (rr. Musculares);
3) the common interosseous artery (a. Interuossea communis), dividing into the anterior and posterior interosseous arteries;
4) deep palmar branch (r. Palmaris profundus);
5) palmar carpal branch (r. Carpalis palmaris).
There are many anastomoses in the subclavian, axillary, brachial, ulnar and radial arteries system, due to which the blood supply to the joints and collateral blood flow are provided.
The branches of the thoracic aorta are subdivided into visceral and parietal.
Visceral branches:
1) pericardial branches (rr. Pericardiaci);
2) esophageal branches (rr. Oesophageales);
3) mediastinal branches (rr. Mediastinaes);
4) bronchial branches (rr. Bronchiales).
Parietal branches:
1) the superior phrenic artery (a.phrenica superior);
2) posterior intercostal arteries (aa. Intercostales posteriores), each of which gives off a medial cutaneous branch (r. Cutaneus medialis), a lateral cutaneous branch (r. Cutaneus lateralis) and a dorsal branch (r. Dorsalis).
9. BRANCHES OF THE ABDOMINAL AORTE
The branches of the abdominal part of the aorta are subdivided into visceral and parietal.
Visceral branches, in turn, are divided into paired and unpaired.
Paired visceral branches:
1) ovarian (testicular) artery (a. Ovarica (a testicularis). The ovarian artery gives tube (rr. Tubarii) and ureteral branches (rr. Ureterici), and the testicular artery - the epididymis (rr. Epididymales) and ureteral branches (rr. ureterici);
2) renal artery (a. Renalis); gives the ureteral branches (rr. ureterici) and the lower adrenal artery (a. suprarenalis inferior);
3) the middle adrenal artery (a. Suprarenalis media); anastomoses with the superior and inferior adrenal arteries.
Unpaired visceral branches:
1) celiac trunk (truncus coeliacus). It is divided into three arteries:
a) splenic artery (a. lienalis), gives branches to the pancreas (rr. pancreatici), short gastric arteries (aa. gastricae breves) and the left gastroepiploic artery (a. gastroepiploica sinistra), giving omental and gastric branches;
b) common hepatic artery (a. hepatica communis); divided into its own hepatic artery (a. hepatica propria) and gastroduodenal artery (a. gastroduodenalis). The own hepatic artery gives off the right gastric artery (a. Gastrica dextra), the right and left branches, the gallbladder artery (a. Cystica) departs from the right branch. The gastroduodenal artery is divided into the upper pancreatoduodenal arteries (aa. Pancreaticoduodenales superiores) and the right gastroepiploic artery (a. Gastroepiploica).
c) the left gastric artery (a. gastrica sinistra), gives off the esophageal branches (rr. oesophagealis);
2) the superior mesenteric artery (a. Mesenterica superior). Gives the following branches:
a) the right colic artery (a. colica dextra); anastomoses with the branches of the middle colon artery, the branch of the ilio-colon artery;
b) the middle colic artery (a. colica media); anastomoses with the right and left colonic arteries;
c) the ilio-colonic artery (a. ileocolica); gives an artery of the appendix (a. appendicularis), a colon-intestinal branch (r. colicus), anterior and posterior cecum arteries (aa. caecalis anterior et posterior);
d) lower pancreatoduodenal arteries (aa. pancreaticoduodenalies inferiors);
e) ileal-intestinal (aa. ileales) and jejunal arteries (aa. jejunales);
3) the lower mesenteric artery (a. Mesenterica inferior). Gives the following branches:
a) sigmoid arteries (aa.sigmoidei);
b) the left colic artery (a. colica sinistra);
c) the superior rectal artery (a. rectalis superior).
Parietal branches:
1) four pairs of lumbar arteries (aa. Lumbales), each of which gives off the dorsal and spinal branches;
2) the lower phrenic artery (a. Phrenica inferior), giving the upper adrenal arteries (aa. Suprarenales superiores).
At the level of the middle of the body of the IV lumbar vertebra, the abdominal part of the aorta is divided into two common iliac arteries, and itself continues into the median sacral artery (a.sacralis mediana).
10. STRUCTURE OF THE BRANCHES OF THE COMMON LIQUID ARTERY
Common iliac artery(a. iliaca communis) is divided into the internal and external iliac arteries at the level of the ilio-sacral articulation.
External iliac artery(a. iliaca externa) gives the following branches:
1) deep artery, circumflex iliac bone (a. Circumflexa iliaca profunda);
2) the lower epigastric artery (a. Epigastrica inferior), giving the pubic branch (r. Pubicus), the cremasteric artery (a. Cremasterica) in men and the artery of the round ligament of the uterus (a. Lig teretis uteri) in women.
Internal iliac artery(a. iliaca interna) gives the following branches:
1) the umbilical artery (a. Umbilicalis), presented in an adult by the medial umbilical ligament;
2) the superior gluteal artery (a. Glutealis superior), which is divided into deep and superficial branches;
3) the lower gluteal artery (a. Glutealis inferior); gives the artery accompanying sciatic nerve(a. comitans nervi ischiadici);
4) the ilio-lumbar artery (a. Iliolumbalis), giving the iliac (r. Iliacus) and lumbar branches (r. Lumbalis);
5) the uterine artery (a. Uterine), giving the tube (r. Tubarius), ovarian (r. Ovaricus) and vaginal branches (rr. Vaginales);
6) the lower urinary artery (a. Vesicalis inferior);
7) lateral sacral arteries (aa.sacrales laterales), giving off the spinal branches (rr.spinales);
8) internal genital artery (a. Pudenda interna); gives the lower rectal artery (a. rectalis inferior) and in women: urethral artery (a. urethralis), dorsal and deep arteries of the clitoris (aa. dorsalis et profunda clitoritidis) and artery of the vestibule bulb (a. bulbi vestibule); in men: urethral artery (a. urethralis), dorsal and deep arteries of the penis (aa. dorsalis et profunda penis), artery of the bulb of the penis (a. bulbi penis);
9) the middle rectal artery (a. Rectalis media);
10) obturator artery (a. Obturatoria); divided into anterior and posterior branches. The latter gives off the acetabular branch (r. Acetabularis). The obturator artery in the pelvic cavity gives off the pubic branch (r. Pubicus).
11. BRANCHES OF THE FEMORAL, PENDANT, ANTERIOR AND PREVIOUS TIBOUS ARTERIES
Femoral artery(a. femoralis) is a continuation of the external iliac artery and gives the following branches:
1) deep artery of the thigh (a. Profunda femoris), giving perforating arteries (aa. Perforantes); the lateral artery, bending around the femur (a. circumflexa femoris lateralis), giving the ascending, transverse and descending branches (rr. ascendens, transversus et descendens); the medial artery, the circumflex of the femur (a.circumflexa femoris medialis), giving the acetabular branch (r. acetabularis) to hip joint, deep and ascending branches (rr.profundus et ascendens);
2) the superficial artery, the circumflex of the ilium (a. Circumflexa iliaca superficialis);
3) superficial epigastric artery (a. Epigastrica superficialis);
4) the descending knee artery (a. Genus descendens); participates in the formation of the knee articular network (rete articulare genus);
5) external genital arteries (aa. Pudendae externae).
Popliteal artery(a. poplitea) is a continuation of the femoral and gives the following branches:
1) the medial lower knee artery (a. Genus inferior medialis); participates in the formation of the knee articular network (rete articulare genus);
2) the lateral lower knee artery (a. Genus inferior lateralis);
3) the medial superior knee artery (a. Genus superior medialis);
4) the lateral superior knee artery (a. Genus superior lateralis);
5) the middle knee artery (a. Genus media).
Anterior tibial artery(ayu tibialis anterior) departs from the popliteal artery in the popliteal fossa and gives the following branches:
1) anterior tibial recurrent artery (a.reccurens tibialis anterior);
2) the posterior tibial recurrent artery (a. Reccurens tibialis posterior);
3) the medial anterior ankle artery (a. Malleolaris anterior medialis);
4) lateral anterior ankle artery (a. Malleolaris anterior lateralis);
5) muscle branches (rr. Musculares);
6) dorsal artery of the foot (a.dorsalis pedis); gives the lateral and medial tarsal arteries (aa.tarsales lateralis et medialis), the arcuate artery (a.arcuata) and is divided into terminal branches: the deep plantar artery (a.plantaris profunda) and the first dorsal metatarsal artery (.a metatarsalis dorsalis I).
Posterior tibial artery(a. tibialis posterior) is a continuation of the popliteal artery and gives the following branches:
1) the medial plantar artery (a. Plantaris medialis), dividing into deep and superficial branches;
2) lateral plantar artery (a. Plantaris lateralis); forms a deep plantar arch (arcus plantaris profundus), from which four plantar metatarsal arteries (aa.metatarsales plantares I-IV) depart. Each metatarsal artery passes into the common plantar digital artery (a. Digitalis plantaris communis), which (except for I) are divided into two own plantar digital arteries (aa. Digitalis plantaris propriae);
3) a branch enveloping the fibula (r. Circumflexus fibularis);
4) peroneal artery (a. Peronea);
5) muscle branches (rr. Musculares).
12. SYSTEM OF UPPER CAVITY VIENNA
Superior vena cava(v. cava superior) collects blood from the veins of the head, neck, both upper extremities, veins of the thoracic and partially abdominal cavities and flows into the right atrium. The azygos vein flows into the superior vena cava on the right, and the mediastinal and pericardial veins on the left. It has no valves.
Unpaired Vienna (v. Azygos) is a continuation into the chest cavity of the right ascending lumbar vein (v. lumbalis ascendens dextra), has two valves in the mouth. The unpaired vein, esophageal veins, mediastinal and pericardial veins, posterior intercostal veins IV-XI and the right superior intercostal veins flow into the azygos vein.
Semi-unpaired vein(v. hemiazygos) is a continuation of the left ascending lumbar vein (v. lumbalis ascendens sinistra). The mediastinal and esophageal veins, an accessory semi-unpaired vein (v. Hemiazygos accessoria), which takes the I-VII upper intercostal veins, the posterior intercostal veins, flow into the semi-unpaired vein.
Posterior intercostal veins(vv. intercostales posteriores) collect blood from the tissues of the walls of the chest cavity and part of the abdominal wall. The intervertebral vein (v. Intervertebralis) flows into each posterior intercostal vein, into which, in turn, the spinal branches (rr. Spinales) and the back vein (v. Dorsalis) flow.
The veins of the spongy substance of the vertebrae and spinal veins flow into the internal anterior and posterior vertebral venous plexuses (plexus venosi vertebrales interni). Blood from these plexuses flows into the accessory semi-unpaired and azygos veins, as well as into the external anterior and posterior vertebral venous plexuses (plexus venosi vertebrales externi), from which blood flows into the lumbar, sacral and intercostal veins and into the accessory semi-unpaired and azygos veins.
Right and left brachiocephalic veins(vv. brachiocephalicae dextra et sinistra) are the roots of the superior vena cava. They have no valves. Collect blood from the upper extremities, organs of the head and neck, upper intercostal spaces. The brachiocephalic veins form when the internal jugular and subclavian veins merge.
Deep cervical vein(v. cervicalis profunda) originates from the external vertebral plexuses and collects blood from the muscles and the auxiliary apparatus of the muscles of the occipital region.
Vertebral vein(v vertebralis) accompanies the artery of the same name, taking blood from the internal vertebral plexuses.
Internal thoracic vein(v. thoracica interna) accompanies the artery of the same name on each side. The anterior intercostal veins (vv. Intercostales anteriores) flow into it, and the roots of the internal thoracic vein are the musculophrenic vein (v. Musculophrenica) and the upper epigastric vein (v. Epigastrica superior).
13. VENINS OF THE HEAD AND NECK
Internal jugular vein(v. jugularis interna) is a continuation of the sigmoid sinus of the hard shell of the brain, has an upper bulb in the initial section (bulbus superior); above the confluence with the subclavian vein is the lower bulb (bulbus inferior). There is one valve above and below the lower bulb. Intracranial tributaries of the internal jugular vein are the eye veins (vv. Ophthalmicae superior et inferior), the veins of the labyrinth (vv. Labyrinthi) and diploic veins.
Through the diploic veins(vv. diploicae): posterior temporal diploic vein (v. diploica temporalis posterior), anterior temporal diploic vein (v. diploica temporalis anterior), frontal diploic vein (v. diploica) and occipital diploic vein (v. diploica occipitalis) - blood flows from the bones of the skull; have no valves. With the help of the emissary veins (vv. Emissariae): the mastoid emissary vein (v. Emissaria mastoidea), the condylar emissary vein (v. Emissaria condylaris) and the parietal emissary vein (v emissaria parietalis) - the diploic veins communicate with the veins of the outer covers of the head.
Extracranial tributaries of the internal jugular vein:
1) the lingual vein (v. Lingualis), which is formed by the deep vein of the tongue, the hyoid vein, the dorsal veins of the tongue;
2) facial vein (v. Facialis);
3) the upper thyroid vein (v. Thyroidea superior); has valves;
4) pharyngeal veins (vv. Pharyngeales);
5) submandibular vein (v. Retromandibularis).
External jugular vein(v. jugularis externa) has paired valves at the level of the mouth and middle of the neck. The transverse veins of the neck (vv. Transversae colli), the anterior jugular vein (v. Jugularis anterior), and the suprascapular vein (v. Suprascapularis) flow into this vein.
Subclavian vein(v. subclavia) unpaired, is a continuation of the axillary vein.
14. THE VEINS OF THE UPPER LIMB. LOWER CAVITY VIENNA SYSTEM. GATE VENA SYSTEM
These veins are represented by deep and superficial veins.
The palmar digital veins fall into the superficial palmar venous arch (arcus venosus palmaris superficialis).
Paired palmar metacarpal veins flow into the deep palmar venous arch (arcus venosus palmaris profundus). Superficial and deep venous arches continue into paired radial and ulnar veins (vv. Radiales et vv palmares), which belong to the deep veins of the forearm. From these veins, two brachial veins (vv. Brachiales) are formed, which merge and form an axillary vein (v. Axillaries), which passes into the subclavian vein.
Superficial veins upper limb .
Dorsal metacarpal veins together with their anastomoses form the dorsal venous network of the hand (rete venosum dorsale manus). The superficial veins of the forearm form a plexus in which the lateral saphenous vein of the hand (v. Cephalica), which is a continuation of the first dorsal metacarpal vein, and the medial saphenous vein of the hand (v. Basilica), which is a continuation of the fourth dorsal metacarpal vein, are isolated. The lateral saphenous vein flows into the axillary vein, and the medial one into one of the brachial veins. Sometimes there is an intermediate vein of the forearm (v. Intermedia antebrachii). The intermediate vein of the elbow (v. Intermedia cubiti) is located in the anterior elbow region (under the skin), has no valves.
There are parietal and visceral tributaries of the inferior vena cava (v. Cava inferior).
Visceral tributaries:
1) renal vein (v. Renalis);
2) adrenal vein (v. Suprarenalis); has no valves;
3) hepatic veins (vv. Hepaticae);
4) ovarian (testicular) vein (v. Ovarica (testicularis)).
Parietal tributaries:
1) lower phrenic veins (vv. Phrenicae inferiors);
2) lumbar veins (vv. Lumbales).
Portal vein(v. portae) is the largest visceral vein, its main tributaries are the splenic vein, superior and inferior mesenteric veins.
Splenic vein(v. lienalis) merges with the superior mesenteric vein and has the following tributaries: the left gastroepiploic vein (v. gastroepiploica sinistra), short gastric veins (vv. gastricae breves) and pancreatic veins (vv. pancreaticae).
Superior mesenteric vein(v. mesenterica superior) has the following tributaries: the right gastroepiploic vein (v. gastroepiploica dextra), the ilio-colon vein (v. ileocolica), the right and middle colic veins (vv. colicae media et dextra), pancreatic veins (vv . pancreaticae), a vein of the appendix (v. appendicularis), veins of the ileum and jejunum (vv. ileales et jejunales).
Inferior mesenteric vein(v. mesenterica inferior) flows into the splenic vein, is formed when the sigmoid veins (vv. sigmoideae), the superior rectal vein (v. rectalis superior) and the left colon vein (v. colica sinistra) merge.
Before entering the gate of the liver, the right and left gastric veins (vv. Gastricae dextra et sinistra), the pre-pyloric vein (v. Prepylorica) and the biliary vein (v. Cystica) flow into the portal vein. Entering the gates of the liver, the portal vein is divided into right and left branches, which in turn are divided into segmental, then into interlobular veins, which extend sinusoidal vessels into the lobules and flow into the central vein. Sublobular veins emerge from the lobules, which merge and form the hepatic veins (vv. Hepaticae).
15. VENINS OF THE PELVIS AND LOWER LIMBS
The right and left common iliac veins (vv. Iliacae communes) form the inferior vena cava.
External iliac vein(v. iliaca externa) unites with the internal iliac vein at the level of the sacroiliac joint and forms the common iliac vein. The external iliac vein receives blood from all veins of the lower limb; has no valves.
The internal iliac vein has visceral and parietal tributaries.
Visceral tributaries:
1) vaginal venous plexus (plexus venosus vaginalis), passing into the uterine venous plexus (plexus venosus uterinus);
2) the prostate venous plexus (plexus venosus prostaticus);
3) urinary venous plexus (plexus venosus vesicalis);
4) rectal venous plexus (plexus venosus rectalis);
5) sacral venous plexus (plexus venosus sacralis).
Parietal tributaries:
1) ilio-lumbar vein (v. Ilicolumbalis);
2) upper and lower gluteal veins (vv. Glutealis superiores et inferiors);
3) lateral sacral veins (vv. Sacrales laterales);
4) obturator veins (vv. Obturatoriae).
Deep veins of the lower limb:
1) femoral vein (v. Femoralis);
2) deep vein of the thigh (v. Femoris profunda);
3) popliteal vein (v. Poplitea);
4) anterior and posterior tibial veins (vv. Tibiales anteriores et posteriores);
5) peroneal veins (vv. Fibulares).
All deep veins (except for the deep vein of the thigh) accompany the arteries of the same name; have many valves.
Superficial veins of the lower extremity:
1) great saphenous vein of the leg (v. Saphena magna); flows into the femoral vein, has many valves. Collects blood from the soles of the feet, anteromedial surface of the lower leg and thigh;
2) small saphenous vein of the leg (v. Saphena parva); flows into the popliteal vein, has many valves. Collects blood from the lateral part of the foot, heel region, saphenous veins of the sole and dorsal venous arch;
3) plantar venous arch (arcus venosus plantares); collects blood from the plantar digital veins; from the arch, blood flows into the posterior tibial veins along the plantar veins (lateral and medial);
4) dorsal venous arch (arcus venosus dorsalis pedis); collects blood from the dorsal digital veins; from the arch the blood flows into the greater and lesser saphenous veins.
There are numerous anastomoses between the systems of the superior and inferior vena cava and the portal vein.
Lecture number 1
Topic: “General questions of anatomy and physiology of the cardiovascular system. Heart, circles of blood circulation ”.
Target: Didactic - to study the structure and types of blood vessels. The structure of the heart.
Lecture plan
Types of blood vessels, features of their structure and function.
The structure, position of the heart.
Circles of blood circulation.
The cardiovascular system consists of the heart and blood vessels and serves for constant blood circulation, lymph outflow, which provides humoral communication between all organs, supply them with nutrients and oxygen and excretion of metabolic products.
Blood circulation is a continuous metabolic condition. When it stops, the body dies.
Teaching about the cardiovascular system is called angiocardiology.
For the first time, an accurate description of the mechanism of blood circulation and the meaning of the heart was given by an English physician - W. Harvey. A. Vesalius - the founder of scientific anatomy - described the structure of the heart. The Spanish doctor - M. Servetus - correctly described the pulmonary circulation.
Types of blood vessels, features of their structure and function
Anatomically, blood vessels are divided into arteries, arterioles, precapillaries, capillaries, postcapillaries, venules, and veins. Arteries and veins are the main vessels, the rest are the microvasculature.
Arteries - vessels carrying blood from the heart, regardless of what kind of blood it is.
Structure:
Most arteries have an elastic membrane between the membranes, which gives the wall elasticity, elasticity.
Types of arteries
Depending on the diameter:
Depending on the location:
Extraorganic;
Intraorgan.
Depending on the structure:
Elastic type - aorta, pulmonary trunk.
Muscular-elastic type - subclavian, general sleepy.
Muscular type - the smaller arteries contribute to their contraction of the movement of blood. A prolonged increase in the tone of these muscles leads to arterial hypertension.
Capillaries - microscopic vessels that are in tissues and connect arterioles with venules (through pre- and postcapillaries). Exchange processes occur through their walls, visible only under a microscope. The wall consists of one layer of cells - the endothelium, located on the basement membrane, formed by loose fibrous connective tissue.
Veins - the vessels that carry blood to the heart, no matter what it is. They consist of three shells:
Inner shell - consists of endothelium.
The middle shell is smooth muscle.
The outer shell is adventitia.
Features of the structure of the veins:
The walls are thinner and weaker.
Elastic and muscle fibers are less developed, so their walls can collapse.
The presence of valves (lunate folds of the mucous membrane) that impede blood flow. Valves do not have: vena cava, portal vein, pulmonary veins, head veins, renal veins.
Anastomoses - branching of arteries and veins; can join and form an anastomosis.
Collaterals - vessels that provide a roundabout outflow of blood bypassing the main one.
The following vessels are functionally distinguished:
The main vessels are the largest - the resistance to blood flow is small.
Resistive vessels (vessels of resistance) are small arteries and arterioles that can alter the blood supply to tissues and organs. They have a well-developed muscular layer, they can narrow.
True capillaries (exchange vessels) - have a high permeability, due to which there is an exchange of substances between blood and tissues.
Capacitive vessels - venous vessels (veins, venules), containing 70-80% of the blood.
Shunting vessels are arteriovenular anastomoses that provide a direct connection between arterioles and venules bypassing the capillary bed.
The cardiovascular system includes two systems:
Circulatory (circulatory system).
Lymphatic.
The structure, position of the heart
Heart - a hollow fibromuscular organ, cone-shaped. Weight - 250-350 g.
Main parts:
The top is facing left and forward.
Base - top and back.
Situated in the anterior mediastinum in the chest cavity.
The upper border is the II intercostal space.
Right - 2 cm medially from the midclavicular line.
Left - from the III rib to the apex of the heart.
Apex of the heart - V intercostal space to the left by 1-2 cm inward from the midclavicular line.
Surfaces:
Sternocostal.
Diaphragmatic.
Pulmonary.
The edges: right and left.
Furrows: coronary and interventricular.
Ears: right and left (additional tanks).
The structure of the heart. The heart has two halves:
The right one is venous.
The left one is arterial.
There are partitions between the halves - the atrial and interventricular.
The heart has 4 chambers - two atria and two ventricles (right and left). The leaflet valves are located between the atria and ventricles. Between the right atrium and the right ventricle there is a tricuspid valve, between the left atrium and the left ventricle there is a bicuspid (mitral) valve.
In the bases of the pulmonary trunk and aorta - semilunar valves. The valves are formed by the endocardium. They prevent blood from flowing back.
Vessels entering and leaving the heart:
Veins flow into the atrium.
The superior and inferior vena cava flow into the right atrium.
4 pulmonary veins flow into the left atrium.
Arteries leave the ventricles.
The aorta emerges from the left ventricle.
The pulmonary trunk leaves the right ventricle and divides into the right and left pulmonary arteries.
Wall structure:
The inner layer - the endocardium - consists of connective tissue with elastic fibers, as well as the endothelium. It forms all the valves.
Myocardium - formed by striated heart tissue (there are bridges between muscle fibers in this tissue).
Pericardium: a) epicardium - fused with the muscularis; b) the pericardium itself, between them - liquid (50 ml). Inflammation - pericarditis.
Circles of blood circulation
Big circle.
It begins with the aorta from the left ventricle and ends with the superior and inferior vena cava that flow into the right atrium.
The exchange of substances between blood and tissues takes place through the walls of the capillaries. Arterial blood gives oxygen to tissues and takes carbon dioxide, becoming venous.
Small circle.
It starts from the right ventricle with the pulmonary trunk and ends with four pulmonary veins that flow into the left atrium.
In the capillaries of the lung, venous blood is enriched with oxygen and becomes arterial.
The crown circle.
It includes the vessels of the heart itself for the blood supply to the heart muscle.
It begins above the aortic bulb with the left and right coronary arteries. They flow into the coronary sinus, which flows into the right atrium.
Flowing through the capillaries, the blood gives oxygen and nutrients to the heart muscle, and receives carbon dioxide and decay products, and becomes venous.
Conclusion.
The human heart is four-chambered, has 4 valves that prevent the reverse flow of blood, 3 membranes.
Function heart - a pump for pumping blood.
Lecture number 2
Topic: "Physiology of the heart".
Target: Didactic - to study the physiology of the heart.
Plan:
Basic physiological properties of the heart muscle.
The work of the heart (cardiac cycle and its phases).
External manifestations of the activity of the heart and indicators of cardiac activity.
Electrocardiogram and its description.
The laws of cardiac activity and regulation of the activity of the heart.
Basic physiological properties of the heart muscle
Excitability.
Conductivity (1-5 m / s).
Contractility.
Refractory period (characterized by a sharp decrease in tissue contractility).
Absolute - during this period, no matter what force irritates, it does not respond to excitations - corresponds in strength to systole and the onset of diastole of the atria and ventricles.
Relative - the excitability of the heart muscle returns to its original level.
Automatism (automaticity) of the heart - the ability of the heart to beat rhythmically regardless of impulses coming from outside. Automation is provided by the conduction system of the heart. This is an atypical, or special, tissue in which arousal arises and is carried out.
Conducting system:
Sinus node - Kisa-Flexa.
Atrioventricular node - Ashof-Tovara.
A bundle of His, which is divided into the right and left legs, passing into the Purkinje fibers.
Finding:
The sinus node is located in the right atrium on the posterior wall at the confluence of the superior vena cava. He is a pacemaker, impulses appear in him that determine the heart rate (60-80 pulses per minute).
The atrioventricular node is located in the right atrium near the septum between the atrium and the ventricles. He is a transmitter of excitement. In pathological conditions (for example, a scar after myocardial infarction) can become a pacemaker (heart rate = 40-60 pulses per minute).
The bundle of His is located in the septum between the ventricles. It is also an excitation transmitter (heart rate = 20-40 pulses per minute).
In pathological conditions, a violation of conductivity occurs.
Heart block - lack of consistency between the rhythm of the atria and ventricles. This leads to severe hemodynamic disturbances.
Fibrillation (flutter and flicker of the heart) - uncoordinated contractions of the muscle fibers of the heart.
Extrasystoles - extraordinary contractions of the heart.
Heart work (cardiac cycle and its phases)
The heart rate in a healthy person is 60-80 beats per minute.
Less than 60 beats per minute - bradycardia.
More than 80 beats per minute - tachycardia.
Heart work - these are rhythmic contractions and relaxation of the atria and ventricles.
Consists of three phases:
Atrial systole and ventricular diastole. In this case, the leaflet valves open, and the semilunar valves close, and the blood of their atria enters the ventricles. This phase lasts 0.1 sec. The blood pressure in the atria rises by 5-8 mm Hg. Art. Thus, the atria mainly play the role of a reservoir.
Ventricular systole and atrial diastole. In this case, the leaf valves are closed, and the semilunar valves are opened. This phase lasts 0.3 sec. The blood pressure in the left ventricle is 120 mm Hg. Art., in the right - 25-30 mm Hg. Art.
General pause (phase of rest and replenishment of the heart with blood). The atria and ventricles relax, the leaflet valves are open, and the semilunar valves are closed. This phase lasts for 0.4 seconds.
The whole cycle is 0.8 sec.
The pressure in the chambers of the heart drops to zero, as a result of which the blood from the hollow and pulmonary veins, where the pressure is 7 mm Hg. Art., flows into the atrium and ventricles by gravity, freely, supplementing about 70% of their volume.
External manifestations of the activity of the heart and indicators of cardiac activity
Apical impulse.
Heart tones.
Electrical phenomena in the heart.
Apical impulse - a beat of the apex of the heart on the chest. It is due to the fact that the heart during ventricular systole turns from left to right and changes its shape: from ellipsoid it becomes round. Visible or palpable in the V intercostal space, 1.5 cm medially from the midclavicular line.
Heart tones - sounds arising from the work of the heart. There are two tones:
I tone - systolic - occurs during the systole of the ventricles and closed leaflet valves. I tone is lower, dull and prolonged.
II tone - diastolic, occurs during diastole and the closure of the semilunar valves. It is shorter and taller.
At rest, with each systole, the ventricles are ejected into the aorta and pulmonary trunk, 70-80 ml - the systolic blood volume. In one minute, up to 5-6 liters of blood are thrown out - the minute volume of blood.
So, for example, if the systolic volume is 80 ml, and the heart contracts to 70 beats per minute, then the minute volume is: 80 * 70 = 5600 ml of blood.
With heavy muscular work, the systolic volume of the heart increases to 180-200 ml, and the minute volume increases to 30-35 l / min.
Electrical properties of the heart
During systole, the atria become electronegative with respect to the ventricles in the diastole phase.
Thus, when the heart works, a potential difference is created, which is recorded by an electrocardiograph.
For the first time, the registration of potentials abroad was carried out using a string galvanometer by V. Einthoven in 1903, and in Russia - by A.F. Samoilov.
The clinic uses three standard leads and chest leads.
In lead I, electrodes are placed on both hands.
In lead II, electrodes are placed on the right arm and left leg.
In lead III, electrodes are placed on the left arm and left leg.
In chest leads, an active positive electrode is applied to certain points of the anterior surface of the chest, and another indifferent combined electrode is formed when three limbs are connected through an additional resistance.
An ECG consists of a series of waves and intervals between them. When analyzing the ECG, the height, width, direction, shape of the teeth are taken into account.
The P wave characterizes the occurrence and spread of excitation in the atria.
The Q wave characterizes the excitation of the interventricular septum.
The R wave covers the excitation of both ventricles.
S wave - completion of excitation in the ventricles.
T - the process of repolarization in the ventricles.
Complexes:
The spread of excitation from the sinus node to the ventricles.
The spread of excitement through the muscles of the ventricles.
General pause.
The ECG is essential for the diagnosis of heart disease.
The laws of cardiac activity and regulation of the activity of the heart
Heart Fiber Law, or Starling's Law - the more a muscle fiber is stretched, the more it contracts.
Law heart rate, or the Beinbridge reflex.
With an increase in blood pressure in the mouths of the vena cava, a reflex increase in the frequency and strength of heart contractions occurs. This is due to the excitation of the mechanoreceptors of the right atrium in the area of the cavity of the vena cava, increased pressure of blood returning to the heart.
Impulses from mechanoreceptors along afferent nerves enter the cardiovascular center of the medulla oblongata, where they reduce the activity of the nuclei of the vagus nerve and increase the influence of sympathetic nerves on the activity of the heart.
These laws work simultaneously, they are referred to as self-regulation mechanisms that ensure the adaptation of the heart to changing conditions of existence.
Lecture number 3
Topic: "Arterial system".
Plan:
Aortic arch.
Blood supply to the brain.
Thoracic aorta.
Abdominal aorta: a) blood supply abdominal cavity(upper floor); b) blood supply to the pelvic organs and lower extremities (lower floor).


Blood supply to the brain
It is carried out by two systems:
I... Vertebral artery system.
The vertebral arteries extend from the subclavian arteries, pass into the openings of the transverse processes of the first 6 cervical vertebrae. They enter the skull through the foramen magnum and in the area of the pons varolian they are connected to the basilar artery. Two posterior cerebral arteries branch off from it, supplying blood to the brain stem. 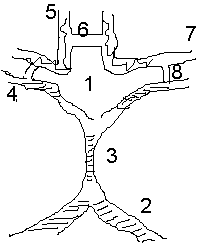
Veliziev circle.
Vertebral arteries.
Basilar artery (in the area of the pons varoli).
Posterior cerebral artery.
Anterior cerebral artery.
Anterior communicating artery.
Middle cerebral artery.
Back connecting.
II... Internal carotid artery system.
The internal carotid arteries enter the skull through the laceration. Gives 3 pairs of branches:
Eye - supply blood to the eyeballs.
The anterior cerebral arteries are interconnected by the anterior communicating arteries.
Middle cerebral - connected to the posterior branches of the posterior connecting arteries.
Lecture number 5
Topic: “Physiology of the vascular system and microcirculation. Lymphatic system ”.
Plan:
The reasons for the movement of blood through the vessels.
Pulse, blood pressure.
Regulation of the heart.
Regulation of vascular tone.
The mechanism of tissue fluid formation.
The lymphatic system.
The patterns of blood flow through the vessels are based on the laws of hydrodynamics.
The reason for the movement of blood through the arteries - the difference in blood pressure at the beginning and end of the circle of blood circulation.
The pressure in the aorta is 120 mm Hg.
The pressure in small arteries is 40-50 mm Hg.
The pressure in the capillaries is 20 mm Hg.
Pressure in large veins - negative or 2-5 mm Hg.
Reasons for the movement of blood through the veins:
The presence of valves.
Contraction of adjacent muscles.
Negative pressure in the chest cavity.
The time of blood flow in the systemic circulation is 20-25 sec.
The time of blood flow in the pulmonary circulation is 4-5 sec.
The cycle time is 20-25 sec.
The speed of movement of blood in the aorta is 0.5 m / sec.
The speed of movement of blood in the arteries is 0.25 m / sec.
The speed of movement of blood in the capillaries is 0.5 mm / sec.
The speed of blood flow in the vena cava is 0.2 m / sec.
Arterial pressure (BP) is the pressure of the blood on 2 vascular walls. Normal - 120/80. The amount of blood pressure depends on three factors:
the magnitude and strength of heart contractions;
peripheral resistance values;
circulating blood volume (BCC).
Distinguish:
systolic pressure;
diastolic pressure;
pulse pressure.
Systolic pressure reflects the state of the left ventricular myocardium.
Diastolic pressure reflects the degree of tone of the arterial walls.
Pulse pressure - the difference between systolic and diastolic pressure.
Blood pressure is measured with a Korotkov tonometer or a Rivo-Rocce tonometer.
Pulse - This is a rhythmic oscillation of the vessel wall due to a systolic increase in pressure in it.
Heart rate characteristics:
rhythm;
filling;
voltage;
sameness (symmetry).
The pulse is felt where the arteries lie close to the bone.
A pulse wave occurs in the aorta at the time of expulsion of blood from the left ventricle. Speed - 6-9 m / sec. The heart works in jerks, and the blood flows in a continuous stream.
Why? During systole, the walls of the aorta stretch and blood flows into the aorta and arteries. During diastole, the walls of the arteries contract. A continuous jet is generated.
The regulation of vascular activity is carried out in two ways: by the nervous and humoral pathways. Nervous regulation of blood circulation is carried out by the vasomotor center, sympathetic and parasympathetic nerves of the autonomic nervous system.
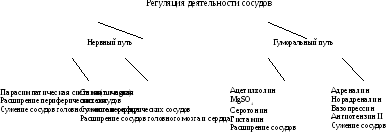
The vasomotor center is a collection of nerve formations located in the spinal cord, medulla oblongata, hypothalamus and cerebral cortex. The main vasomotor center is located in the medulla oblongata and consists of two sections: pressor and depressor. Irritation of the first section leads to vasoconstriction, the second - to their expansion.
The vasomotor center exerts its influence through sympathetic neurons spinal cord, then to the sympathetic nerves and blood vessels and causes their constant tonic tension. The tone of the vasomotor center of the medulla oblongata depends on nerve impulses coming to it from various reflexogenic zones.
Reflexogenic zones are areas of the vascular wall containing the largest number of receptors.
Mechanoreceptors - baroreceptors, perceiving fluctuations in blood pressure 1-2 mm Hg.
Chemoreceptors - perceive changes in the chemical composition of the blood (CO2, O2, CO).
Volumoreceptors - perceive a change in the BCC.
Osmoreceptors - perceive changes in osmotic blood pressure.
Reflexogenic zones:
Aortic (aortic arch).
Sinocarotid (common carotid artery).
The very heart.
The mouth of the hollow veins.
The area of the vessels of the pulmonary circulation.
Pressure change, chemical composition sensitively perceived by receptors, and information enters the central nervous system.
Let us consider this on the basis of the depressor and pressor reflexes.
Depressive reflex
It occurs due to an increase in blood pressure in the blood vessels. In this case, the baroreceptors of the aortic arch and the carotid sinus are excited, from which the excitation of the depressor nerve enters the vasomotor center of the medulla oblongata. This leads to a decrease in the activity of the pressor center and an increase in the inhibitory effect of the fibers of the vagus nerve. The result is vasodilation and bradycardia.

Pressor reflex
It is observed with a decrease in blood pressure in the vascular system.
In this case, the function of impulses coming from the aortic and carotid zones along the sensory nerves decreases sharply, which leads to inhibition of the center of the vagus nerve and an increase in the tone of sympathetic innervation. At the same time, blood pressure rises, blood vessels are narrowed.
Reflex Meaning: Maintain a constant level of blood pressure in the vessels and prevent the possibility of its excessive increase. They are called “blood pressure relievers”.
Humoral substances affecting blood vessels:
vasoconstrictor - adrenaline, norepinephrine, vasopressin, renin;
vasodilators - acetylcholine, histamine, K, Mg ions, lactic acid.
Physiology of microcirculation
Microcirculatory bed - this is blood circulation in the system of capillaries, arterioles and venules.
Capillary - this is the final link of the microvasculature, here the exchange of substances and gases takes place between the blood and the cells of the tissues of the body through the intercellular fluid.
Capillary Is a thin tube with a length of 0.3-0.7 mm.
The length of all capillaries is 100,000 km. At rest, 10-25% of the capillaries function. Blood flow velocity - 0.5-1 mm / sec. The pressure at the arterial end is 35-37 mm Hg, at the venous end - 20 mm Hg.
Exchange processes in the capillaries, i.e., the formation of intercellular fluid, is carried out in two ways:
by diffusion;
by filtration and reabsorption.
Diffusion - the movement of molecules from an environment with a high concentration to an environment where the concentration is lower. From blood into tissues diffuse: Na, K, Cl, glucose, amino acids, O 2. From tissues diffuse: urea, CO 2 and other substances.
Diffusion is facilitated by: the presence of pores, windows and gaps. The diffusion volume is 60 l / min, that is, 85,000 l per day.
Filtration and reabsorption mechanism
, providing exchange, is carried out due to the difference between the hydrostatic pressure of the blood in the capillaries and the oncotic pressure in the interstitial fluid. 
Filtration volume - 14 ml / min.
The volume of reabsorption is 12 ml / min.
Thus, the volume per day is 18 liters.
9. Right atrium
10. Right ventricle
11. Left atrium
12. Left ventricle
13. Trabeculae
15. Tricuspid valve
16. Mitral valve
17. Pulmonary valve
In order to talk about diseases of the cardiovascular system, it is necessary to imagine its structure. Circulatory system divided into arterial and venous. Through the arterial system, blood flows from the heart, through the venous system - flows to the heart. Distinguish between a large and a small circle of blood circulation.
The large circle includes the aorta (ascending and descending, aortic arch, thoracic and abdominal), through which blood flows from the left heart. From the aorta, blood enters the carotid arteries that supply blood to the brain, subclavian arteries, blood supplying arms, renal arteries, arteries of the stomach, intestines, liver, spleen, pancreas, pelvic organs, iliac and femoral arteries, blood supplying legs. From the internal organs, blood flows through the veins, which flow into the superior vena cava (collects blood from the upper half of the body) and the inferior vena cava (collects blood from the lower half of the body). The vena cava flows into the right heart.
The pulmonary circulation includes the pulmonary artery (through which, however, venous blood flows). Through the pulmonary artery, blood enters the lungs, where it is enriched with oxygen and becomes arterial. Through the pulmonary veins (four), arterial blood enters the left heart.
The heart pumps blood - a hollow muscular organ consisting of four sections. It is the right atrium and right ventricle that make up the right heart and the left atrium and left ventricle that make up the left heart. Oxygen-rich blood flowing from the lungs through the pulmonary veins enters the left atrium, from it - into the left ventricle and further into the aorta. Venous blood through the superior and inferior vena cava enters the right atrium, from there into the right ventricle and then through the pulmonary artery into the lungs, where it is enriched with oxygen and again enters the left atrium.
Distinguish between pericardium, myocardium and endocardium. The heart is located in the heart sac - the pericardium. Cardiac muscle - the myocardium consists of several layers of muscle fibers, there are more of them in the ventricles than in the atria. These fibers, by contracting, push blood from the atria to the ventricles and from the ventricles to the vessels. The internal cavities of the heart and valves are lined by the endocardium.
Heart valve apparatus
Between the left atrium and the left ventricle there is a mitral (bicuspid) valve, between the right atrium and the right ventricle there is a tricuspid (tricuspid) valve. The aortic valve is located between the left ventricle and the aorta, the pulmonary valve is between the pulmonary artery and the right ventricle.
Heart work
From the left and right atrium, blood flows into the left and right ventricles, while the mitral and tricuspid valves are open, the aortic and pulmonary valves are closed. This phase in the work of the heart is called diastole. Then the mitral and tricuspid valves close, the ventricles contract, and through the opened aortic and pulmonary artery valves, blood, respectively, rushes into the aorta and pulmonary artery. This phase is called systole; systole is shorter than diastole.
Conductive system of the heart
We can say that the heart works autonomously - it itself generates an electrical impulse that spreads through the heart muscle, forcing it to contract. The impulse should be generated with a certain frequency - normally about 50-80 impulses per minute. In the conducting system of the heart, a sinus node is distinguished (located in the right atrium), nerve fibers go from it to the atrioventricular (atrioventricular) node (located in the interventricular septum - the wall between the right and left ventricles). From the atrioventricular node, nerve fibers go in large bundles (right and left leg of His), dividing in the walls of the ventricles into smaller ones (Purkinje fibers). An electrical impulse is generated in the sinus node and propagates along the conductive system in the thickness of the myocardium (heart muscle).
Blood supply to the heart
Like all organs, the heart must receive oxygen. Oxygen is delivered through arteries called coronary arteries. The coronary arteries (right and left) depart from the very beginning of the ascending aorta (at the site of the origin of the aorta from the left ventricle). The trunk of the left coronary artery is divided into the descending artery (aka the anterior interventricular artery) and the circumflex artery. These arteries give off branches - an artery of a blunt edge, diagonal, etc. Sometimes the so-called median artery departs from the trunk. The branches of the left coronary artery supply blood to the anterior wall of the left ventricle, most of the interventricular septum, the lateral wall of the left ventricle, and the left atrium. The right coronary artery supplies a portion of the right ventricle and the posterior wall of the left ventricle.
Now that you have become a specialist in the anatomy of the cardiovascular system, let's move on to its diseases.
Thromboembolism is a blockage of blood vessels by blood clots. The most dangerous is thromboembolism of the pulmonary artery and its branches.
Peripheral artery disease:
- Arterial stenosis and occlusion
- Arterial aneurysms
- Raynaud's disease (syndrome)
- Diseases of peripheral veins
- Thrombosis of peripheral veins
Natural science. Lectures + Experiments
About the program
The best Russian teachers conduct fascinating classes in physics, chemistry and biology for TV viewers, illustrating the lectures with the most interesting experiments.
Yuri Olesha in "Three Fat Men" described one of his heroes, Dr. Gaspar Arneri, in verses:
"How to fly from the ground to the stars,
The best Russian teachers - this time precisely those scientists who know "how to make steam out of stone" - read lectures on physics, chemistry and biology to viewers. And also - they conduct the most interesting and informative experiments on these subjects.
Anatomy of the vascular system
AORTA
The aorta is subdivided into ascending part(pars aortae ascendens), arc(arcus aortae) and descending part(pars descendens aortae), consisting of the thoracic and abdominal regions. From the aortic arch, there are arteries involved in the blood supply to the brain and upper limbs (brachiocephalic trunk, left common carotid and left subclavian arteries). The brachiocephalic trunk is divided into the right common carotid and subclavian arteries. In the carotid triangle, the common carotid artery is divided into external and internal. The external carotid artery and its branches supply blood to most of the face and neck. The internal carotid artery on the neck does not branch out, goes steeply upward, through the carotid canal it penetrates into the cranial cavity to the base of the brain. The vertebral arteries branch off from the subclavian arteries. The vertebral artery enters the cranial cavity through the foramen magnum. At the base of the brain, the internal carotid and vertebral arteries form an arterial ring (circle of Willis). The subclavian arteries continue into the axillary arteries. The axillary artery passes into the brachial artery, the terminal branches of which are the radial and ulnar arteries. They, in turn, give rise to smaller branches that provide blood supply to the hand.
Abdominal aorta gives off branches that supply blood to the gastrointestinal tract (celiac trunk, superior and inferior mesenteric arteries), kidneys (renal arteries) and lower limbs (right and left common iliac arteries). The common iliac artery is divided into the internal and external iliac arteries. The external iliac artery continues into the femoral artery, the largest branch of which is the deep thigh artery, extending from its lateral surface below the inguinal ligament. In the popliteal fossa, the femoral artery passes into the popliteal artery, which divides into the anterior and posterior tibial arteries. The latter gives rise to the peroneal artery. The terminal branches of these three arteries of the lower leg provide blood supply to the foot.
ARTERIES
The walls of the arteries consist of three sheaths: outer, or adventitia (tunica externa), middle (tunica media) and inner (tunica intima). Adventitia is formed by loose connective tissue. The middle shell is represented by several layers of circularly located smooth muscle fibers, among which there is a network of elastic fibers that form a common frame of the arterial wall with elastic elements of the adventitia and intima. The intima of the artery is formed by the endothelium, the basement membrane and the subendothelial layer, which includes thin elastic fibers and stellate cells. Behind it is a network of thick elastic fibers that form an internal elastic membrane. Depending on the predominance of certain morphological elements in the vessel walls, arteries of elastic, muscular and mixed types are distinguished.
Blood supply the walls of the arteries are carried out by their own arterial and venous vessels (vasa vasorum). Intima has no blood vessels.
Innervation arteries are provided by the sympathetic and parasympathetic nervous systems. An important role in the regulation of vascular tone belongs to chemo-, baro- and mechanoreceptors located in a large number in the walls of arteries, especially in the bifurcation zone of the common carotid artery (carotid sinus zone).
Capillaries
A direct continuation of the arterial network is the microcirculation system, which unites vessels with a diameter of 2-100 microns. Each morphological unit of the microcirculatory system includes 5 elements: 1) arteriole; 2) precapillary arteriole; 3) capillary; 4) postcapillary venule and 5) venule. In the microcirculatory bed, transcapillary exchange takes place, which ensures the vital functions of the body. It is carried out on the basis of filtration, reabsorption, diffusion and microvesicular transport. Filtration takes place in the arterial section of the capillary, where the sum of the values of the hydrostatic pressure of the blood and the osmotic pressure of the plasma is on average 9 mm Hg. Art. exceeds the value of the oncotic pressure of tissue fluid. In the venous section of the capillary, there is an inverse relationship between the values of these pressures, which contributes to the reabsorption of the interstitial fluid with metabolic products. Based on this, any pathological processes accompanied by increased permeability of the capillary wall for protein lead to a decrease in oncotic pressure, and, consequently, to a decrease in reabsorption.
VIENNA
Distinguish superficial and deep veins limbs. Superficial veins of the lower extremities represented by the large and small saphenous veins. The greater saphenous vein (v. Saphena magna) starts from the inner marginal vein of the foot, is located in the depression between the anterior edge of the medial ankle and the tendons of the flexor muscles and rises along the inner surface of the lower leg and thigh to the oval fossa, where at the level of the lower horn of the crescent edge of the broad fascia the thigh flows into the femoral vein. The small saphenous vein (v. Saphena parva) is a continuation of the lateral marginal vein of the foot, begins in the depression between the lateral ankle and the edge of the achilles tendon and rises along the posterior surface of the leg to the popliteal fossa, where it falls into the popliteal vein. There are many anastomoses between the small and large saphenous veins on the lower leg.
The deep venous network of the lower extremities is presented paired veins... accompanying the arteries of the fingers, feet, lower leg. The anterior and posterior tibial veins form a non-paired popliteal vein that passes into the trunk of the femoral vein. One of the major tributaries of the latter is the deep vein of the thigh. At the level of the lower edge of the inguinal ligament, the femoral vein passes into the external iliac vein, which, merging with the internal iliac vein, gives rise to the common iliac vein. The latter merge to form the inferior vena cava.
The connection between the superficial and deep venous systems is carried out by communicating (perforating or perforating) veins. Distinguish between direct and indirect communication veins. The first of them directly connect the saphenous veins with the deep ones, the latter carry out this connection through the small venous trunks of the muscle veins. Direct communicating veins are located mainly along the medial surface of the lower third of the leg (Cockett's vein group), where there are no muscles, as well as along the medial surface of the thigh (Dodd's group) and the lower leg (Boyd's group). Usually, the diameter of the perforating veins does not exceed 1–2 mm. They are equipped with valves that normally direct blood flow from superficial veins to deep ones. In case of insufficiency of the valves, there is an abnormal blood flow from deep veins to superficial ones.
VENINS OF THE UPPER LIMBS
The superficial veins of the upper limb include the subcutaneous venous network of the hand, the medial saphenous vein (v.basilica) and the lateral saphenous vein of the hand (v.cephalica). V. basilica, being a continuation of the veins of the back of the hand, rises along the medial surface of the forearm, shoulder and flows into the brachial vein (v. Brachialis). V.cephalica is located laterally
the edge of the forearm, shoulder and flows into the axillary vein (v.axillaris).
Deep veins are represented by paired veins accompanying the arteries of the same name. The radial and ulnar veins flow into the two brachial veins, which in turn form the axillary vein trunk. The latter continues into the subclavian vein, which, merging with the internal jugular vein, forms the brachiocephalic vein (v. Brachicephalica). From the confluence of the brachiocephalic veins, the trunk of the superior vena cava is formed.
VENINS OF LOWER LIMBS
The veins of the lower extremities have valves that facilitate the movement of blood in the centripetal direction, preventing its reverse flow. At the confluence of the great saphenous vein into the femoral vein, there is an osteal valve that restrains the backflow of blood from the femoral vein. Along the great saphenous and deep veins, there are a significant number of such valves. The movement of blood in the centripetal direction is facilitated by the difference between the relatively high pressure in the peripheral veins and the low pressure in the inferior vena cava. Systolic-diastolic vibrations of the arteries, transmitted to nearby veins, and the "suction" action of the diaphragm's respiratory movements, which lowers the pressure in the inferior vena cava during inspiration, also contribute to the advancement of blood in the centripetal direction. An important role is also played by the tone of the venous wall.
VENOUS PRESSURE
An important role in the implementation of the return of venous blood to the heart is played by the muscle-venous pump of the lower leg. Its components are the venous sinuses of the gastrocnemius muscles (sural veins), in which a significant amount of venous blood is deposited, the gastrocnemius muscles, which squeeze out with each contraction and push the venous blood into the deep veins, venous valves that prevent the reverse flow of blood. The essence of the mechanism of action of the venous pump is as follows. At the moment of relaxation of the leg muscles ("diastole"), the sinuses of the soleus muscle are filled with blood coming from the periphery and from the superficial venous system through the perforating veins. With each step, there is a contraction of the calf muscles, which compresses the muscular venous sinuses and veins ("systole"), directing the blood flow to the deep main veins, which have big number valves all over. Under the influence of increasing venous pressure, the valves open, directing blood flow into the inferior vena cava. Downstream valves close, preventing backflow.
The blood pressure in the vein depends on the height of the hydrostatic (the distance from the right atrium to the foot) and the hydraulic pressure of the blood (equivalent to the gravitational component). In the vertical position of the body, the hydrostatic pressure in the veins of the legs and feet increases sharply and is added to the lower hydraulic pressure. Normally, venous valves contain the hydrostatic pressure of the blood column and prevent overstretching of the veins.
About 85% of the blood volume is located in the venous system (capacitive vessels), which takes part in the regulation of the circulating blood volume in various pathological conditions. Thermoregulation of the body largely depends on the tone and degree of filling of cutaneous venules, subdermal venous plexuses and saphenous veins. The superficial vein system provides heat exchange between the body and the environment through vasoconstriction and vasodilation of the veins.
Anatomy and physiology of the heart: structure, functions, hemodynamics, cardiac cycle, morphology
The structure of the heart of any organism has many characteristic nuances. In the process of phylogenesis, that is, the evolution of living organisms to more complex ones, the heart of birds, animals and humans acquires four chambers instead of two chambers in fish and three chambers in amphibians. Such a complex structure is best suited for the separation of arterial and venous blood flows. In addition, the anatomy of the human heart implies many smallest details, each of which performs its strictly defined functions.
Heart as an organ
So, the heart is nothing more than a hollow organ, consisting of specific muscle tissue, which carries out the motor function. The heart is located in the chest behind the sternum, more on the left, and its longitudinal axis is directed anteriorly, to the left and down. In front, the heart is bordered by the lungs, almost completely covered by them, leaving only a small part directly adjacent to the chest from the inside. The boundaries of this part are otherwise called absolute cardiac dullness, and they can be determined by tapping the chest wall ().
In people with a normal constitution, the heart has a semi-horizontal position in the chest cavity, in people with an asthenic constitution (thin and tall) - almost vertical, and in hypersthenics (dense, stocky, with a large muscle mass) - almost horizontal.

position of the heart
The posterior wall of the heart is adjacent to the esophagus and to the large main vessels (to the thoracic aorta, to the inferior vena cava). The lower part of the heart is located on the diaphragm.
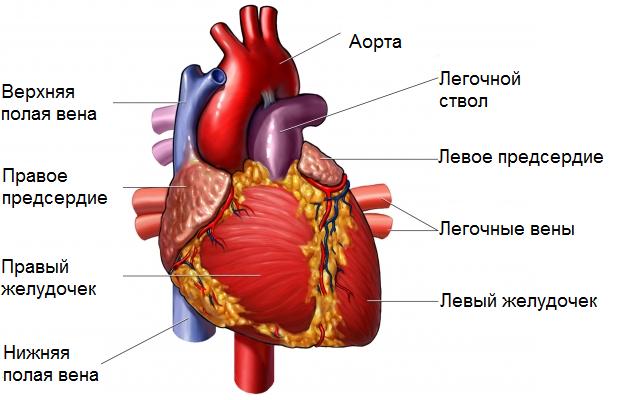
external structure of the heart
Age features
The human heart begins to form in the third week of the prenatal period and the entire period of gestation continues, passing through the stages from a single-chamber cavity to a four-chambered heart.

intrauterine heart development
The formation of four chambers (two atria and two ventricles) occurs already in the first two months of pregnancy. The smallest structures are fully formed for childbirth. It is in the first two months that the heart of the embryo is most vulnerable to the negative influence of certain factors on the expectant mother.
The heart of the fetus participates in the blood flow through its body, but differs in the circulatory system - the fetus does not yet have its own breathing with its lungs, but it “breathes” through the placental blood. There are some openings in the fetal heart that allow pulmonary blood flow to be “turned off” from the circulation prior to delivery. During childbirth, accompanied by the first cry of the newborn, and, therefore, at the time of an increase in intrathoracic pressure and pressure in the baby's heart, these openings are closed. But this does not always happen, and they can remain in the child, for example, (should not be confused with such a defect as an atrial septal defect). An open window is not a heart defect, and subsequently, as the child grows, it overgrows.

hemodynamics in the heart before and after birth
The heart of a newborn baby has a rounded shape, and its dimensions are 3-4 cm in length and 3-3.5 cm in width. In the first year of a child's life, the heart increases significantly in size, and more in length than in width. The heart mass of a newborn baby is about 25-30 grams.
As the baby grows and develops, the heart also grows, sometimes significantly outstripping the development of the body itself according to age. By the age of 15, the mass of the heart increases almost tenfold, and its volume increases more than fivefold. The heart grows most intensively until the age of five, and then during puberty.
In an adult, the size of the heart is about 11-14 cm in length and 8-10 cm in width. Many people rightly believe that the size of the heart of each person corresponds to the size of his clenched fist. The weight of the heart in women is about 200 grams, and in men - about 300-350 grams.
After 25 years, changes begin in the connective tissue of the heart, which forms the heart valves. Their elasticity is no longer the same as in childhood and adolescence, and the edges may become uneven. As a person grows up and then ages, changes occur in all structures of the heart, as well as in the vessels that feed it (in the coronary arteries). These changes can lead to the development of numerous cardiac diseases.
Anatomical and functional features of the heart
Anatomically, the heart is an organ divided by septa and valves into four chambers. The "upper" two are called the atria (atrium), and the "lower" two are called the ventricles (ventriculum). The atrial septum is located between the right and left atria, and the interventricular septum is located between the ventricles. Normally, these partitions do not have holes in them. If there are holes, this leads to mixing of arterial and venous blood, and, accordingly, to hypoxia of many organs and tissues. Such holes are called baffle defects and are referred to as.

basic structure of the chambers of the heart
The boundaries between the upper and lower chambers are the atrioventricular openings - the left one, covered by the cusps of the mitral valve, and the right one, covered by the cusps of the tricuspid valve. The integrity of the septa and the correct functioning of the valve leaflets prevent mixing of blood flows in the heart, and contribute to a clear unidirectional movement of blood.
The atria and ventricles are different - the atria are smaller than the ventricles, and the walls are thinner. So, the wall of the atria is about only three millimeters, the wall of the right ventricle is about 0.5 cm, and the left one is about 1.5 cm.
The atria have small protrusions - ears. They have a slight suction function for better pumping of blood into the atrial cavity. The mouth of the vena cava flows into the right atrium near its ear, and four (less often five) pulmonary veins into the left atrium. From the ventricles there is a pulmonary artery (more commonly called the pulmonary trunk) on the right and the aortic bulb on the left.

the structure of the heart and the vessels included in it
From the inside, the upper and lower chambers of the heart are also different and have their own characteristics. The surface of the atria is smoother than that of the ventricles. From the valve ring between the atrium and the ventricle, thin connective tissue valves originate - bicuspid (mitral) on the left and tricuspid (tricuspid) on the right. The other edge of the cusps is turned into the ventricles. But so that they do not hang freely, they are, as it were, supported by thin tendon threads called chords. They are like springs, stretching when the valve cusps are closed and compressed when the cusps open. Chords originate from the papillary muscles from the wall of the ventricles - in the composition of three in the right and two in the left ventricle. That is why the ventricular cavity has an uneven and bumpy inner surface.
The functions of the atria and ventricles also differ. Due to the fact that the atria need to push blood into the ventricles, and not into the larger and longer vessels, they have to overcome the resistance of the muscle tissue less, therefore the atria are smaller in size and their walls are thinner than those of the ventricles. The ventricles push blood into the aorta (left) and into pulmonary artery(on right). Conventionally, the heart is divided into right and left halves. The right half serves for the flow of exclusively venous blood, and the left half serves for arterial blood. Schematically, "right heart" is indicated in blue, and "left heart" - in red. Normally, these streams never mix.

hemodynamics in the heart
One cardiac cycle lasts about 1 second and is carried out as follows. At the moment of filling the atria with blood, their walls relax - atrial diastole occurs. The valves of the vena cava and pulmonary veins are open. The tricuspid and mitral valves are closed. Then the atrial walls tighten and push blood into the ventricles, the tricuspid and mitral valves open. At this point, systole (contraction) of the atria and diastole (relaxation) of the ventricles occur. After the blood has been taken by the ventricles, the tricuspid and mitral valves close, and the valves of the aorta and pulmonary artery open. Further, the ventricles are already contracted (ventricular systole), and the atria are again filled with blood. There comes a general diastole of the heart.

cardiac cycle
The main function of the heart is reduced to pumping, that is, to push a certain blood volume into the aorta with such pressure and speed that blood is delivered to the most distant organs and to the smallest cells of the body. Moreover, arterial blood with a high content of oxygen and nutrients is pushed into the aorta, which enters the left half of the heart from the vessels of the lungs (flows to the heart through the pulmonary veins).
Venous blood, low in oxygen and other substances, is collected from all cells and organs from the vena cava system, and flows into the right half of the heart from the superior and inferior vena cava. Further, venous blood is pushed from the right ventricle into the pulmonary artery, and then into the pulmonary vessels in order to carry out gas exchange in the alveoli of the lungs and in order to enrich with oxygen. In the lungs, arterial blood is collected in the pulmonary venules and veins, and again flows into the left half of the heart (into the left atrium). And so the heart regularly pumps blood through the body at a frequency of 60-80 beats per minute. These processes are denoted by the concept "Circles of blood circulation". There are two of them - small and large:
- Small circle includes the flow of venous blood from the right atrium through the tricuspid valve into the right ventricle - then into the pulmonary artery - then into the arteries of the lungs - enrichment of blood with oxygen in the pulmonary alveoli - the flow of arterial blood into the smallest veins of the lungs - into the pulmonary veins - into the left atrium.
- Big circle includes the flow of arterial blood from the left atrium through the mitral valve into the left ventricle - through the aorta into the arterial bed of all organs - after gas exchange in tissues and organs, the blood becomes venous (with a high content of carbon dioxide instead of oxygen) - further into the venous bed of organs - into the hollow system veins - in the right atrium.

circles of blood circulation
Video: Anatomy of the Heart and Cardiac Cycle in Brief
Morphological features of the heart
If you look at slices of the heart under a microscope, you can see a special type of muscle that is no longer found in any other organ. This is a type of striated muscle, but with significant histological differences from ordinary skeletal muscles and from the muscles lining the internal organs. The main function of the heart muscle, or myocardium, is to provide the most important ability of the heart, which is the basis of the life of the whole organism as a whole. It is the ability to contract, or contractility.In order for the fibers of the heart muscle to contract synchronously, electrical signals must be supplied to them, which excite the fibers. This is another ability of the heart — .
Conduction and contractility are possible due to the fact that the heart autonomously generates electricity in itself. These functions (automatism and excitability) are provided by special fibers, which are an integral part of the conductive system. The latter is represented by electrically active cells of the sinus node, atrio-ventricular node, the bundle of His (with two legs - right and left), as well as Purkinje fibers. In the case when a patient's myocardial damage affects these fibers, they develop, otherwise called.
cardiac cycle
Normally, an electrical impulse originates in the cells of the sinus node, which is located in the area of the right atrial appendage. In a short period of time (about half a millisecond), the impulse propagates through the atrial myocardium, and then enters the cells of the atrioventricular junction. Typically, signals are transmitted to the AV node through three main paths - the Wenckenbach, Torel and Bachmann beams. In the cells of the AV node, the time of impulse transmission is lengthened to 20-80 milliseconds, and then the impulses pass through the right and left legs (as well as the anterior and posterior branches of the left leg) of the His bundle to the Purkinje fibers, and, as a result, to the working myocardium. The frequency of transmission of impulses along all the pathways is equal to the heart rate and is 55-80 impulses per minute.
So, the myocardium, or heart muscle, is the middle sheath in the wall of the heart. The inner and outer membranes are connective tissue and are called the endocardium and epicardium. The last layer is part of the pericardial bag, or cardiac "shirt". A cavity is formed between the inner layer of the pericardium and the epicardium, filled with a very small amount of fluid, to ensure better sliding of the layers of the pericardium at the moments of heart contractions. Normally, the volume of fluid is up to 50 ml, exceeding this volume may indicate pericarditis.
![]()
structure of the heart wall and shell
Blood supply and innervation of the heart
Despite the fact that the heart is a pump for providing the whole body with oxygen and nutrients, it itself also needs arterial blood. In this regard, the entire wall of the heart has a well-developed arterial network, which is represented by the branching of the coronary (coronary) arteries. The mouths of the right and left coronary arteries extend from the root of the aorta and are subdivided into branches that penetrate into the thickness of the heart wall. If these important arteries become clogged with blood clots and atherosclerotic plaques, the patient will develop and the organ will no longer be able to perform its functions in full.
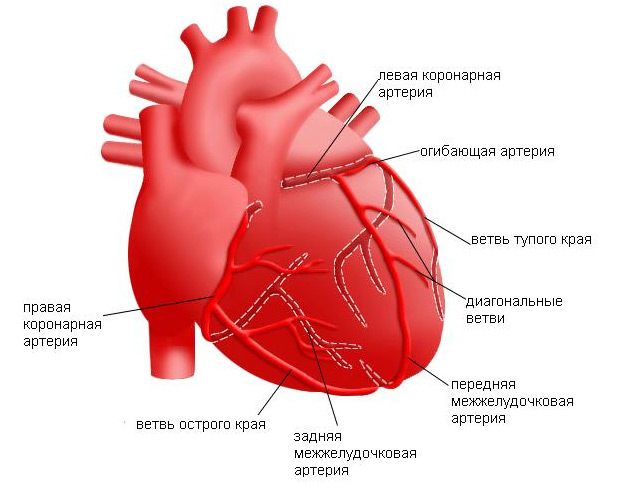
the location of the coronary arteries that supply the heart muscle (myocardium)
The frequency and strength with which the heart beats is influenced by nerve fibers extending from the most important nerve conductors - the vagus nerve and the sympathetic trunk. The first fibers have the ability to slow down the rate of the rhythm, the last - to increase the frequency and strength of the heartbeat, that is, they act like adrenaline.
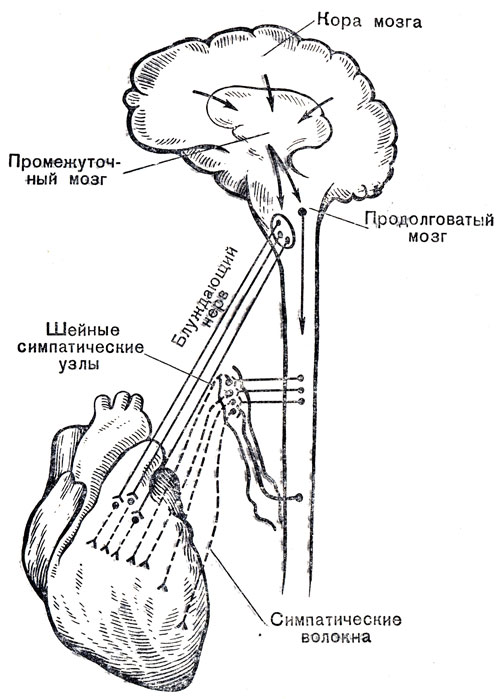
innervation of the heart
In conclusion, it should be noted that the anatomy of the heart may have any deviations in individual patients, therefore, only a doctor is able to determine the norm or pathology in a person after an examination, who is able to visualize the cardiovascular system in the most informative way.
Video: lecture on heart anatomy
