There are 13 pairs of cranial nerves: 0 pair - terminal nerve, n. terminalis; I- olfactory, n. оlfactorius; II- visual, n. opticus; III - oculomotor, n. oculomotorius; IV- block, n. trochlearis; V - trigeminal, n. trigeminus; VI - diverting, n. abducens; VII - front, n. facialis; Vjjj - vestibular-cochlear, n. vestibulocochlearis; IX - glossopharyngeal, n. glossofaryngeus; X - wandering, n. vagus; XI - additional, n. accessorius; XII - sublingual, n. hypoglossus.
DEVELOPMENT AND PRINCIPLES OF THE STRUCTURE OF THE CRANIAL NERVES
The olfactory and optic nerves - specific nerves of the sensory organs, develop from the forebrain and are its outgrowths. The rest of the cranial nerves have differentiated from the spinal nerves and therefore are fundamentally similar in structure to them. Differentiation and transformation of primary spinal nerves in the cranial are associated with the development of the sense organs and branchial arches with the muscles belonging to them, as well as with the reduction of myotomes in the head region (Fig. 227). However, none of the cranial nerves corresponds completely to the spinal nerves, since it is not composed of the anterior and posterior roots, but only of one anterior or posterior one. Cranial nerves jjj, jV, Vj correspond to the anterior roots. Their nuclei are located ventrally; they innervate the muscles that have developed from the 3 anterior somites of the head. The rest of the anterior roots are reduced.
Other cranial nerves: V, Vjj, Vjjj, X, Xj and Xjj can be viewed as dorsal root homologues. These nerves are associated with muscles that have differentiated from the musculature of the branchial apparatus and developed from the lateral plates of the mesoderm. The nerves form two branches - anterior and posterior. In higher vertebrates, the posterior ramus is usually reduced.
Rice. 227. Cranial nerves of the human embryo.
The branchial arches are marked with Arabic numerals, the nerves with Roman numerals.
Some cranial nerves (X, Xjj) have a complex origin, as they are formed by the fusion of several spinal nerves. In connection with the assimilation of the metameres of the trunk by the occipital region of the head, part of the spinal nerves move cranially and enter the region of the medulla oblongata. The cranial nerves jX and Xj developed from a common source - the primary vagus nerve and are, as it were, its branches (Table 14).
Table 14. Correlation of somites of the head, branchial arches and cranial nerves with their roots


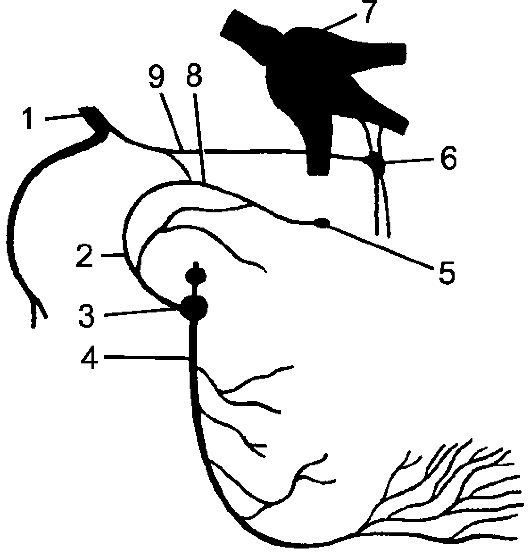
Rice. 228. Connections IX, X and XI pairs of cranial nerves.
1 - diamond-shaped fossa; 2 - spinal cord; 3 - branches from the lower node of the vagus nerve to the sympathetic trunk; 4 - the superior laryngeal nerve; 5 - the lower node of the vagus nerve; 6 - the outer branch of the accessory nerve; 7 - an internal branch of the accessory nerve; 8 - the upper node of the vagus nerve; 9 - lower node of the glossopharyngeal nerve; 10 - a long branch of the vagus nerve; 11 - the upper node of the glossopharyngeal nerve; 12 - cranial roots of the accessory nerve; 13 - the vagus nerve; 14 - glossopharyngeal nerve.
The cranial nerves are distributed according to functional affiliation as follows. Somatic-sensitive nerves include pairs I, II, VIII, somatic-motor - III, IV, VI, XI, XII pairs, mixed, containing somatic-motor and visceral-sensory fibers (VII, IX, X pairs), as well as visceral motor fibers - V, VII, IX, X pairs.
V, VI, VII, VIII, IX, X, XI, XII pairs are connected with the diamond-shaped brain; with the midbrain - jjj and jV pairs; with an intermediate - j and II pairs of cranial nerves (Fig. 228).
0 PAIR - TERMINAL NERVES
Terminal nerve (0 pair), n. terminalis are a pair of small nerves that are closely attached to the olfactory nerves. For the first time they were
found in lower vertebrates, but their presence has been shown in human fetuses and in adults. They contain many myelin-free fibers and associated small groups of bipolar and multipolar nerve cells. Each nerve runs along the medial side of the olfactory tract, their branches pierce the ethmoid plate of the ethmoid bone and branch out in the nasal mucosa. Centrally, the nerve is connected to the brain near the anterior perforation and the septal region. Its function is unknown, but it is thought to represent the head of the sympathetic nervous system, which extends to the blood vessels and glands of the nasal mucosa.
I PAIR - OLFACTOR NERVES
Olfactory nerven. olfactorius, formed by 15-20 olfactory filaments, fila olfactoria, which consist of nerve fibers - processes of olfactory cells located in the mucous membrane of the upper part of the nasal cavity. The olfactory filaments enter the cranial cavity through an opening in the ethmoid plate and end at the olfactory bulbs, which continue into the olfactory tract, tractus olfactorius(see p. 650).
II PAIR - OPTICAL NERVES
Optic nerven. opticus, consists of nerve fibers formed by the processes of multipolar nerve cells of the retina of the eyeball. The optic nerve forms in the posterior hemisphere of the eyeball and passes in the orbit to the optic canal, from where it exits into the cranial cavity. Here, in the precross furrow, both optic nerves are connected, forming the optic chiasm, chiasma opticum. The continuation of the visual tract is called the optic tract, tractus opticus. In the optic chiasm, the medial group of nerve fibers of each nerve passes into the optic tract of the opposite side, and the lateral group continues into the corresponding optic tract. The optic tracts reach the subcortical visual centers.
III PAIR - ORAL MOTOR NERVES
Oculomotor nerven. oculomotorius, mainly motor, arises in the motor nucleus, nucleus n. oculomotorius, Wednesday

Rice. 229. Orbital nerves; side view.
1 - oculomotor nerve; 2 - abducent nerve; 3, 9 - maxillary nerve; 4 - the upper branch of the oculomotor nerve; 5 - nasal nerve; 6 - frontal nerve; 7 - mandibular nerve; 8 - optic nerve; 10 - pterygopalatine node; 11 - ciliary node; 12 - the lower branch of the oculomotor nerve; 13 - short ciliary nerves; 14 - infraorbital nerve.
his brain and parasympathetic accessory nucleus, nucleus accessorius. It extends to the base of the brain at the medial edge of the cerebral peduncle and goes forward in the upper wall of the cavernous sinus to the superior orbital fissure, through which it enters the orbit and divides into the superior branch, r. superior, - to the upper rectus muscle and muscle lifting the eyelid, and the lower branch, r. inferior, - to the medial and lower straight and lower oblique muscles. A branch departs from the lower branch to the ciliary node, which is its parasympathetic root (Fig. 229).
IV PAIR - BLOCK NERVES
Block nerven. trochlearis, motor, originates in the motor nucleus, nucleus n. trochlearis, located in the midbrain at the level of the lower colliculus. It goes out to the base of the brain outward from the bridge and continues forward in the outer wall of the cavernous

Rice. 230. Trigeminal nerve.
1 - trigeminal node; 2 - optic nerve; 3 - the maxillary nerve; 4 - mandibular nerve; 5 - the bottom of the jV ventricle; 6 - lingual nerve; 7 - nerves to the masticatory muscles.
th sine. Through the superior orbital fissure it flows into the orbit and branches into the superior oblique muscle.
V PAIR - TRIPLE NERVES
Trigeminal nerve,n. trigeminus, is mixed and contains motor and sensory nerve fibers. It innervates the chewing muscles, the skin of the face and the anterior part of the head, the hard shell of the brain, as well as the mucous membranes of the nasal and oral cavities, teeth.
The trigeminal nerve has a complex structure. It is distinguished: 1) nuclei (1 motor and 3 sensitive); 2) sensitive and motor roots; 3) the trigeminal node on the sensitive root; 4) the trunk of the trigeminal nerve; 5) 3 main branches of the trigeminal nerve: ocular, maxillary and mandibular nerves(fig. 230).
Sensory nerve cells, the neurites of which form the sensitive branches of the trigeminal nerve, are located in the trigeminal ganglion, ganglion trigeminale. The trigeminal knot overlies the trigeminal depression, impressio trigeminale, the anterior surface of the pyramid of the temporal bone in the trigeminal cavity, cavum trigeminale, formed by the cleavage of the dura mater. The knot is flat, semi-moon-shaped, 14-29 mm long and 5-10 mm high. In people with a brachycephalic skull, it is short and tall, and in dolichocephalics, it is long and low.
The trigeminal ganglion cells are pseudo-unipolar and give off one process, which is divided into 2 near the cell body: central and peripheral. Central neurites form sensitive root,radix sensoria, and through it they enter the brain stem, reaching the sensitive nerve nuclei: bridge core,nucleus pontinus n. trigemini, in the bridge, spinal(lower nucleus of the trigeminal nerve), nucleus spinalis (inferior) n. trigemini, - in the lower part of the cerebral bridge and in the medulla oblongata, as well as the nucleus of the middle cerebral tract,nucleus mesencephalicus n. trigemini, - in the midbrain. Peripheral dendrites are part of the listed main branches of the trigeminal nerve.
Motor nerve fibers originate in motor nucleus of the nerve,nucleus motorius n. trigemini, lying at the back of the bridge. These fibers leave the brain and form motor root,radix motoria. The exit site of the motor root from the brain and the entrance of the sensory root is located at the transition of the bridge to the middle cerebellar peduncle. There are often (in 25% of cases) anastomotic connections between the sensory and motor roots of the trigeminal nerve, as a result of which a number of nerve fibers pass from one root to another.
The diameter of the sensory root is 2.0-2.8 mm, it contains from 75,000 to 150,000 myelin nerve fibers with a diameter of mainly up to 5 microns. The thickness of the motor root is less - 0.8-1.4 mm. It contains from 6,000 to 15,000 myelin nerve fibers with a diameter, usually more than 5 microns.
The sensory root with the trigeminal node belonging to it and the motor root together make up the trunk of the trigeminal nerve with a diameter of 2.3-3.1 mm, containing from 80,000 to 165,000 myelin nerve fibers. Motor root
bypasses the trigeminal node and is part of the mandibular nerve.
Parasympathetic nerve nodes are associated with the 3 main branches of the trigeminal nerve: the ciliary node - with optic nerve, pterygopalatine - with the maxillary, ear and submandibular nodes - with the mandibular nerves.
The general plan of branching of the ophthalmic branches of the trigeminal nerve is as follows: each nerve (ophthalmic, maxillary and mandibular) gives off a branch to the dura mater; internal branches to the mucous membrane of the accessory sinuses, oral and nasal cavities and organs (lacrimal gland, eyeball, salivary glands, teeth); external branches: medial - to the skin of the anterior areas of the face and lateral - to the skin of the lateral areas of the face.
EYE NERVE
Optic nerven. ophthalmicus, is the first, thinnest branch of the trigeminal nerve. Functionally, the nerve is predominantly sensitive. It innervates the skin of the forehead and the anterior part of the temporal and parietal regions, the upper eyelid, the back of the nose, and also partially the mucous membrane of the nasal cavity, the shell of the eyeball and the lacrimal gland (Fig. 231).
The nerve is 2-3 mm thick, consists of 30-70 relatively small bundles and contains from 20,000 to 54,000 myelinated nerve fibers, mostly of small diameter (up to 5 microns). Upon departure from the trigeminal node, the nerve passes in the outer wall of the cavernous sinus, where it gives off thin branches to the oculomotor, block and abducent nerves, a branch of the tentacle, r. tentorius, to the outline of the cerebellum and takes several branches from the internal carotid plexus. Near the superior orbital fissure, the optic nerve is divided into 3 branches: the lacrimal, frontal and nasal ciliary nerves (Fig. 232).
1. Lacrimal nerven. lacrimalis, located near the outer wall of the orbit, where it connects connecting branch with zygomatic nerve, r. communicans cum n. zygomatico. It innervates the lacrimal gland, as well as the skin of the upper eyelid and the lateral angle of the palpebral fissure.
2. Frontal nerven. frontalis, - the thickest branch of the optic nerve. It passes under the upper wall of the orbit and is divided into two branches: supraorbital nerven. supraorbitalis, going through the supraorbital notch to the skin of the forehead, and supra block nerve,n. supratrochlearis, going out-

Rice. 231. The optic nerve.
from the orbit at its inner wall and innervating the skin of the upper eyelid and the medial corner of the eye.
3. Nasal nerve.n. nasociliaris, lies in the orbit near its medial wall and under the block of the superior oblique muscle leaves the orbit in the form of a terminal branch - subblock nerve,n. infratrochlearis, which innervates the lacrimal sac, conjunctiva and the medial corner of the eye. Throughout its length, the nasal nerve gives off the following branches: 1) long ciliary nerves, pp. ciliares longi, to the eyeball; 2) posterior ethmoidal nerve, item ethmoidalis posterior, to the mucous membrane of the sphenoid sinus and posterior cells of the ethmoid labyrinth; 3) anterior ethmoidal nerve, item ethmoidalis anterior, to the mucous membrane of the frontal sinus and nasal cavity (rr. nasales medialis et lateralis) and to the skin of the tip and wing of the nose. In addition, a connecting branch departs from the nasal nerve to the ciliary node.
Ciliary nodeganglion ciliare(Fig. 233), up to 2 mm long, lies on the lateral surface of the optic nerve, approximately on the border between the posterior and middle third of the orbit length. In the ciliary node, as in other parasympathetic nodes of the trigeminal nerve, there are parasympathetic multifaceted (multipolar) nerve cells, on which preganglionic fibers, forming synapses, switch to postganglionic ones. Sympathetic and sensory fibers pass through the node in transit.

Rice. 232. Orbital nerves; view from above.
1 - muscle lifting the upper eyelid; 2 - the lacrimal gland; 3 - superior rectus muscle; 4 - the lacrimal nerve; 5 - lateral rectus muscle; 6 - middle cranial fossa; 7 - temporal muscle; 8 - lateral pterygoid muscle; 9 - mandibular nerve; 10 - accessory nerve; 11 - the vagus nerve; 12 - glossopharyngeal nerve; 13 - the cochlear part of the vestibular cochlear nerve; 14 - the vestibular part of the vestibular cochlear nerve; 15 - facial nerve; 16 - abducent nerve; 17 - trigeminal nerve; 18, 25 - trochlear nerve; 19 - trigeminal nerve; 20 - the oculomotor nerve; 21 - internal carotid artery; 22 - maxillary nerve; 23 - optic nerve; 24 - optic nerve; 26 - superior oblique muscle; 27 - lattice plate; 28 - nasal nerve; 29 - cock's comb; 30 - supraorbital nerve; 31 - frontal nerve; 32 - block; 33 - frontal sinus.
Connecting branches in the form of its roots are suitable for the node: 1) sensitive, radix nasociliaris, - from the nasal nerve; 2) parasympathetic, radix oculomotoris, - from the oculomotor nerve; 3) sympathetic, radix sympathicus, - from the plexus surrounding a. ophthalmica. From the ciliary node departs from 4 to 10 short

Rice. 233. Ciliary node (diagram).
1 - white connecting branch; 2 - upper cervical node of the sympathetic trunk; 3 - internal sleepy plexus; 4 - sympathetic root; 5 - ciliary node; 6 - nasal root; 7 - the oculomotor nerve; 8 - oculomotor root; 9 - short ciliary nerves; 10 - preganglionic parasympathetic fibers; 11 - postganglionic parasympathetic fibers; 12 - sensitive fibers; 13 - postganglionic sympathetic fibers; 14 - sympathetic nucleus; 15 - spinal nerve; 16 - preganglionic sympathetic fibers; 17 - motor fibers.
ciliary nerves, pp. ciliares breves, going inside the eyeball. They contain postganglionic parasympathetic fibers innervating the ciliary muscle and the sphincter of the pupil, sensory fibers innervating the membranes of the eyeball, as well as sympathetic fibers to the muscle that dilates the pupil.
The maxillary nerve
Maxillary nerven. maxillaris, - the second branch of the trigeminal nerve, mostly sensitive. It has a thickness of 2.5-4.5 mm and consists of 25-70 small bundles containing from 30,000 to 80,000 myelinated nerve fibers, mostly of small diameter (up to 5 microns).
The maxillary nerve innervates the dura mater of the brain, the skin of the lower eyelid, the lateral angle of the eye, the anterior part of the temporal region, the upper part of the cheek, the wings of the nose, the skin and mucous membrane of the upper lip, the mucous membrane of the posterior and lower parts of the nasal cavity, the mucous membrane of the sphenoid sinus, palate , the teeth of the upper jaw (Fig. 234). Upon exiting the skull through the round opening, the nerve enters the pterygo-palatine fossa, passes from back to front and from the inside to the outside. The length of the segment and its position in the fossa depend on the shape of the skull. With a brachycephalic skull, the length of the nerve segment in the fossa is 15-22 mm, it is located deep in the fossa - up to 5 cm from the middle of the zygomatic arch. Sometimes the nerve in the pterygo-palatine fossa is closed with a bone crest. With a dolichocephalic skull, the length of the nerve section under consideration is 10-15 mm, and it is located more superficially - up to 4 cm from the middle of the zygomatic arch.
Within the pterygo-palatine fossa, the maxillary nerve gives meningeal branch, r. meningeus, to the dura mater and is divided into 3 branches: 1) the nodal branches going to the pterygopalatine node, 2) the zygomatic nerve and 3) the infraorbital nerve, which is a direct continuation of the maxillary nerve.
1. Nodal branches,rr. ganglionares, number 1-7, depart from the maxillary nerve at a distance of 1.0-2.5 mm from the round opening and go to the pterygopalatine node, giving out sensory fibers to the nerves starting from the node. Some nodal branches bypass the node and join its branches.
Pterygopalatine knot,ganglion pterygopalatinum, - the formation of the parasympathetic part of the autonomic nervous system. Triangular node, 3-5 mm long, contains multipolar cells
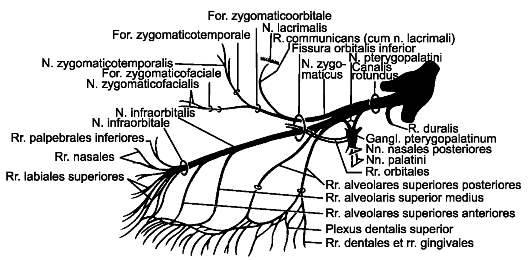
Rice. 234. Maxillary nerve.
and has 3 roots: 1) sensitive - nodal branches,nn. pterygopalatini; 2) parasympathetic - large stony nerve,n. petrosus major(a branch of the intermediate nerve), contains fibers to the glands of the nasal cavity, palate, lacrimal gland; 3) sympathetic - deep stony nerve,n. petrosus profundus, departs from the internal carotid plexus, contains postganglionic sympathetic nerve fibers from the cervical nodes. Branches depart from the node, which include secretory (parasympathetic and sympathetic) and sensory fibers (Fig. 235):
1) orbital branches,rr. orbitales, 2-3 thin trunks, penetrate through the lower orbital fissure and then, together with the posterior ethmoid nerve, go through the small openings of the sphenoid-ethmoid suture to the mucous membrane of the posterior cells of the ethmoid labyrinth and the sphenoid sinus;
2) posterior superior nasal branches,rr. nasales posteriores superiores, 8-14 in number leave the pterygo-palatine fossa through the wedge-palatine opening into the nasal cavity and are divided into two groups: lateral and medial. Lateral branches, rr. nasales posteriores superiores laterales(6-10), go to the mucous membrane of the posterior portions of the superior and middle turbinates and nasal passages, posterior cells of the ethmoid bone, the superior surface of the choanas and the pharyngeal opening of the auditory tube. Medial branches, rr. nasales posteriores superiores mediales(2-3), branch in the mucous membrane of the upper section

Rice. 235. Pterygopalatine node (diagram).
1 - maxillary nerve; 2 - preganglionic parasympathetic fibers of the large stony nerve; 3 - postganglionic sympathetic fibers of the deep stony nerve; 4 - palatine nerves; 5 - postganglionic parasympathetic fibers; 6 - zygomatic nerve; 7 - the connecting branch of the zygomatic and lacrimal nerves; 8 - the lacrimal nerve; 9 - lacrimal gland; 10 - the nerve of the pterygoid canal; 11 - nodal branches of the maxillary nerve; 12 - posterior nasal nerves; 13 - sensitive fibers.
septum of the nose. One of the medial branches - nasopalatine nerve
n. nasopalatinus, passes between the periosteum and the mucous membrane of the septum together with the posterior artery of the nasal septum forward, to the nasal opening of the incisal canal, through which it reaches the mucous membrane of the anterior part of the palate. Forms a connection with the nasal branch of the superior alveolar nerve (Fig. 236).
Palatine nervesnn. palatini, spread from the node through the great palatine canal, forming 3 groups of nerves:
1) great palatine nerve,n. palatinus major, - the thickest branch, goes through the large palatine opening to the palate, where it splits into 3-4 branches, innervating most of the mucous membrane of the palate and its glands in the area from the canines to the soft palate;

Rice. 236. Olfactory nerve, pterygopalatine ganglion and branches of the trigeminal nerve. 1 - lower nasal passage; 2, 4, 7 - inferior, middle and superior turbinates, respectively; 3 - middle nasal passage; 5 - olfactory bulb; 6 - olfactory nerves; 8 - sphenoid sinus; 9 - optic nerve; 10, 23 - internal carotid artery; 11 - the oculomotor nerve; 12 - pterygopalatine node; 13 - optic nerve; 14 - the maxillary nerve; 15 - trigeminal node; 16 - the nerve of the pterygoid canal; 17 - trigeminal nerve; 18 - large stony nerve; 19 - deep stony nerve; 20, 31 - facial nerve; 21 - vestibular cochlear nerve; 22 - internal carotid nerve plexus; 24 - lingual nerve; 25 - lower alveolar nerve; 26 - drum string; 27 - middle meningeal artery; 28 - maxillary artery; 29 - subulate process; 30 - mastoid process; 32 - parotid salivary gland; 33 - perpendicular plate of the palatine bone; 34 - medial pterygoid muscle; 35 - palatine nerves; 36 - soft palate; 37 - hard palate; 38 - upper lip.
2) small palatine nerves,nn. palatini minores, enter the oral cavity through the small palatine openings and branch out in the mucous membrane of the soft palate and the area of the palatine tonsil;
3) lower posterior nasal branches,rr. nasales posteriores inferiores, enter the great palatine canal, leave it through small openings and enter the nasal cavity at the level of the inferior turbinate, innervating the mucous membrane of the inferior concha, middle and lower nasal passages and maxillary sinus.
2. Zygomatic nerven. zygomaticus, Branches from the maxillary nerve within the pterygo-palatine fossa and penetrates through the lower orbital fissure into the orbit, where it goes along the outer wall, exits through the zygomatic-orbital foramen and is divided into two branches:
1) zygomaticofacial branch,r. zygomaticofacialis, comes out through the zygomatic opening to the anterior surface of the zygomatic bone, in the skin of the upper part of the cheek gives off a branch to the area of the outer corner of the palpebral fissure and a connecting branch to the facial nerve;
2) zygomatic branch,r. zygomaticotemporalis, leaves the orbit through the opening of the zygomatic bone of the same name, pierces the temporal muscle and its fascia and innervates the skin of the anterior part of the temporal and posterior part of the frontal regions. Gives the connecting branch to the lacrimal nerve, containing secretory parasympathetic fibers to the lacrimal gland.
3. Infraorbital nerven. infraorbitalis, is a continuation of the maxillary nerve and gets its name from the departure from the last previously mentioned branches. The infraorbital nerve leaves the pterygo-palatine fossa through the inferior orbital fissure, passes along the inferior wall of the orbit together with the vessels of the same name in the infraorbital groove (in 15% of cases, there is a bony canal instead of a groove) and exits through the infraorbital foramen under the muscle that lifts the upper lip, dividing to the final branches. The length of the infraorbital nerve is different: in brachycephalics, the trunk of the nerve is 20-27 mm, and in dolichocephals - 27-32 mm. The position of the nerve in the orbit corresponds to the parasagittal plane drawn through the infraorbital foramen.
The nature of branch branching can also be different: loose, in which numerous thin nerves with a large number of connections depart from the trunk, or trunk nerves with a small number of large nerves. On its way, the infraorbital nerve gives off the following branches:
1) upper alveolar nerves,nn. alveolares superiores, innervate the teeth and the upper jaw (Fig. 237). There are 3 groups of branches of the superior alveolar nerves:
a) posterior superior alveolar branches, rr. alveolares superiores posteriores, branch off from the infraorbital nerve, as a rule, in the pterygo-palatine fossa in number 4-8 and are located together with the vessels of the same name on the surface of the tubercle of the upper jaw. Some of the posterior nerves go along the outer surface of the tubercle down to the alveolar process, the rest enter through the posterior
![]()
Rice. 237. Maxillary nerve.
1 - posterior upper alveolar branches; 2 - zygomatic nerve; 3 - the maxillary nerve; 4 - the nerve of the pterygoid canal; 5 - optic nerve; 6 - trigeminal nerve; 7 - mandibular nerve; 8 - drum string; 9 - ear node; 10 - connecting branches of the pterygopalatine node with the maxillary nerve; 11 - chewing nerve; 12 - lower alveolar nerve; 13 - lingual nerve; 14 - pterygopalatine node; 15 - infraorbital nerve; 16 - anterior superior alveolar branches.
upper alveolar openings in the alveolar canals. Branching together with other upper alveolar branches, they form a nervous upper dental plexus,plexus dentalis superior, which lies in the alveolar process of the upper jaw above the apex of the roots. The plexus is quite dense, wide-looped, stretched along the entire length of the alveolar process. The upper gingival branches extend from the plexus, rr. gingivales superiores, to the periodontium and periodontium in the area of the upper molars, and the upper dental branches, rr. dentales superiores, to the tops of the roots of the large molars, in the pulp cavity of which they branch. In addition, the posterior superior alveolar branches send fine nerves to the maxillary sinus mucosa;
b) middle upper alveolar branch, r. alveolaris superior medius, in the form of one or, less often, two trunks it branches off from the infraorbital nerve, more often in the pterygo-palatine fossa and less often within the orbit, passes in one of the alveolar canals and branches into
bony tubules of the upper jaw as part of the upper dental plexus. Has connecting branches with posterior and anterior superior alveolar branches. Innervates through the upper gingival branches the periodontium and the periodontium in the area of the upper premolars, through the upper dental branches - the upper premolars;
v) anterior superior alveolar branches, rr. alveolares superiores anteriores, arise from the infraorbital nerve in the anterior part of the orbit, which they leave through the alveolar canals, penetrating into the anterior wall of the maxillary sinus, where they are part of the upper dental plexus. The upper gingival branches innervate the mucous membrane of the alveolar process and the walls of the alveoli in the area of the upper canines and incisors, the upper dental branches - the upper canines and incisors. The anterior superior alveolar branches send the thin nasal ramus to the mucous membrane of the anterior fundus of the nasal cavity;
2) lower branches of the eyelids,rr. palpebrales inferiores, branch off from the infraorbital nerve at the exit from the infraorbital foramen, penetrate the muscle that lifts the upper lip, and, branching out, innervate the skin of the lower eyelid;
3) external nasal branches,rr. nasales externi, innervate the skin in the wing of the nose;
4) internal nasal branches,rr. nasales interni, fit to the mucous membrane of the vestibule of the nasal cavity;
5) upper lip branches,rr. labiales superiores, 3-4, go between the upper jaw and the muscle that lifts the upper lip down; innervate the skin and mucous membrane of the upper lip to the corner of the mouth.
All of the listed external branches of the infraorbital nerve form connections with the branches of the facial nerve.
The lower maxillary nerve
Mandibular nerven. mandibularis, - the third branch of the trigeminal nerve is a mixed nerve and is formed by sensory nerve fibers coming from the trigeminal ganglion and motor fibers of the motor root. The thickness of the trunk of the nerve ranges from 3.5 to 7.5 mm, and the length of the extracranial section of the trunk is 0.5-2.0 cm. The nerve consists of 30-80 bundles of fibers, including from 50,000 to 120,000 myelinated nerve fibers.
The mandibular nerve carries out the sensitive innervation of the hard membrane of the brain, the skin of the lower lip, chin, lower cheek, anterior part of the auricle and external auditory canal, part of the surface of the tympanic membrane, the mucous membrane of the cheek, the floor of the mouth and the anterior two-thirds of the tongue, teeth lower jaw, as well as the motor innervation of all the masseter muscles, the maxillary-hyoid muscle, the anterior abdomen of the digastric muscle and the muscles that strain the eardrum and the palatine curtain.
From the cranial cavity, the mandibular nerve exits through the foramen ovale and enters the infratemporal fossa, where it is divided near the exit site into a series of branches. Branching of the mandibular nerve is possible or loose type(more often in dolichocephalic) - the nerve splits into many branches (8-11), or trunk type(more often in brachycephalic) with branching into a small number of trunks (4-5), which are common to several nerves.
Three nodes of the autonomic nervous system are associated with the branches of the mandibular nerve: ear,ganglion oticum;submandibular,ganglion submandibulare;sublingual,ganglion sublinguale. Postganglionic parasympathetic secretory fibers go from the nodes to the salivary glands.
The mandibular nerve gives off a number of branches (Fig. 238, 239).
1. Meningeal branchr. meningeus, passes through the spinous foramen together with the middle meningeal artery into the cranial cavity, where it branches into the hard shell.
2. Chewing nerven. massetericus, predominantly motor, often (especially with the main form of branching of the mandibular nerve) has a common origin with other nerves of the masticatory muscles. It passes outwardly over the upper edge of the lateral pterygoid muscle through the notch of the lower jaw and is introduced into the masseter muscle. Before entering the muscle, it sends a thin branch to the temporomandibular joint, providing its sensitive innervation.
3. Deep temporal nervesnn. temporales profundi, motor, pass along the outer base of the skull outward, bend around the infratemporal ridge and enter the temporal muscle from its inner surface in the anterior (n. temporalis profundus anterior) and back (item temporalis profundus posterior) departments.

Rice. 238. The structure of the mandibular nerve.
3. Lateral pterygoid nerve,n. pterygoideus lateralis, motor, usually departs from the common trunk with the buccal nerve, approaches the muscle of the same name, in which it branches.
4. Medial pterygoid nerven. pterygoideus medialis, mainly motor. It passes through the ear node or adjoins its surface and follows forward and downward to the inner surface of the muscle of the same name, into which it penetrates near its upper edge. In addition, near the ear node gives off n. tensoris tympani, n. tensoris veli palatini and a connecting branch to the node.
5. Buccal nerven. buccalis, sensitive, penetrates between the two heads of the lateral pterygoid muscle and goes along the inner surface of the temporal muscle, spreading further along with the buccal vessels along the outer surface of the buccal muscle to the corner of the mouth. On its way, it gives off thin branches that pierce the buccal muscle and innervate the mucous membrane of the cheek (up to the gums of the 2nd premolar and 1st molar) and branches to the skin of the cheek and corner of the mouth. Forms a connecting branch with the branch of the facial nerve and with the ear node.

Rice. 239. Mandibular nerve.
1 - maxillary nerve; 2 - the superior alveolar nerve; 3, 4 - infraorbital nerve; 5 - buccal nerve; 6 - buccal muscle: 7, 10 - lower alveolar nerve; 8 - chewing muscle (cut off and turned away); 9 - lingual nerve; 11 - lateral pterygoid muscle; 12 - chewing nerve; 13 - facial nerve; 14 - auricular nerve; 15 - temporal muscle.
6. Ear-temporal nerve,n. auriculotemporalis, sensitive, starts from the posterior surface of the mandibular nerve with two roots, covering the middle meningeal artery, which are then connected to a common trunk. Gives the connecting branch to the ear node. Near the neck of the articular process of the lower jaw, the ear-temporal nerve goes up and through the parotid salivary gland goes into the temporal region, where it branches into terminal branches - superficial temporal, r. temporales superficiales. On its way, the ear-temporal nerve gives off the following branches:
1) articular,r. articulares, to the temporomandibular joint;
2) parotid,r. parotidei, to the parotid gland. These branches contain, in addition to sensitive, parasympathetic secretory fibers from the ear node;
3) nerve of the external auditory canal,n. meatus acustici externi, to the skin of the external auditory canal and eardrum;
4) anterior ear nervesn. auriculares anteriores, to the skin of the anterior part of the auricle and the middle part of the temporal region.
7. Lingual nerven. lingualis, sensitive. It originates from the mandibular nerve near the foramen ovale and is located between the pterygoid muscles anterior to the inferior alveolar nerve. At the upper edge of the medial pterygoid muscle or somewhat lower, it joins the nerve drum string,chorda tympani, which is a continuation of the intermediate nerve. As part of the drum string, secretory fibers are included in the lingual nerve, following to the submandibular and hypoglossal nerve nodes, and taste fibers to the papillae of the tongue. Further, the lingual nerve passes between the inner surface of the lower jaw and the medial pterygoid muscle, over the submandibular salivary gland along the outer surface of the sublingual muscle to the lateral surface of the tongue. Between the hyoid-lingual and chin-lingual muscles, the nerve disintegrates into the terminal lingual branches, rr. linguales.
In the course of the nerve, connecting branches are formed with the hypoglossal nerve and the tympanic string. In the oral cavity, the lingual nerve gives off the following branches:
1) branches of the throat isthmus,rr. isthmi faucium, innervating the mucous membrane of the pharynx and the posterior floor of the oral cavity;
2) hypoglossal nerven. sublingualis, departs from the lingual nerve at the posterior edge of the hyoid node in the form of a thin connecting branch and extends forward along the lateral surface of the hyoid salivary gland. Innervates the mucous membrane of the floor of the mouth, the gums and the sublingual salivary gland;
3) lingual branches,rr. linguales, pass along with the deep artery and veins of the tongue through the muscles of the tongue forward and end in the mucous membrane of the apex of the tongue and its body along the borderline. As part of the lingual branches, taste fibers pass to the papillae of the tongue, passing from the drum string.
8. Lower alveolar nerve,n. alveolaris inferior, mixed. It is the largest branch of the mandibular nerve. The trunk lies between the pterygoid muscles behind and lateral to the lingual nerve, between the mandible and the sphenoid-mandibular ligament. The nerve enters, together with the vessels of the same name, into the mandibular canal, where it gives off multiple branches that anastomose with each other and form lower dental plexus,plexus dentalis inferior(in 15% of cases), or directly the lower teeth
ny and gingival branches. It leaves the canal through the chin foramen, dividing before entering the chin nerve and the incisal branch. Sends out the following branches:
1) jaw-hypoglossal nerve, and. mylohyoideus, occurs near the entrance of the lower alveolar nerve into the mandibular opening, is located in the groove of the same name of the mandibular branch and goes to the maxillary-hyoid muscle and the anterior abdomen of the digastric muscle;
2) lower dental and gingival branches,rr. dentales et gingivales inferiores, originate from the inferior alveolar nerve in the mandibular canal; innervate the gums, alveoli of the alveolar part of the jaw and teeth (premolars and molars);
3) chin nerven. mentalis, is a continuation of the trunk of the lower alveolar nerve at the exit through the chin opening from the canal of the lower jaw, where the nerve is divided fan-like into 4-8 branches, among which there are: a) chin, rr. mentales, to the skin of the chin; b) lower labial, rr. labiates inferiores, to the skin and mucous membrane of the lower lip.
Ear node,ganglion oticum, - rounded body with a diameter of 3-5 mm; located under the oval opening on the posteromedial surface of the mandibular nerve. It is approached by the small petrosal nerve (from the glossopharyngeal), which brings the preganglionic parasympathetic fibers. A number of connecting branches depart from the node: 1) to the ear-temporal nerve, into which the postganglionic parasympathetic secretory fibers enter, which then go as part of the parotid branches to the parotid salivary gland; 2) to the meningeal branch, containing fibers supplying the vessels of the dura mater of the brain; 3) to the drum string; 4) to the pterygopalatine and trigeminal nodes (Fig. 240).
Submandibular nodeganglion submandibulare, the size of 3.0 - 3.5 mm, is located under the trunk of the lingual nerve and is associated with the nodal branches, rr. ganglionares. Along these branches, the fibers of the drum string go to the node and end there. The postganglionic branches departing from the node innervate the submandibular and sublingual salivary glands (see Fig. 235).
Sometimes (up to 30% of cases) there is a separate sublingual node,ganglion sublinguale.
VI PAIR - abducens nerves
Abducens nerve n. abducens- motor. The nucleus of the abducens nerve,nucleus n. abducentis, located in front of the bottom of the IV ventricle. The nerve leaves the brain at the posterior

Rice. 240. Ear and submandibular nodes (diagram).
1 - mandibular nerve; 2, 10 - preganglionic parasympathetic fibers; 3 - small stony nerve; 4 - the connecting branch of the ear node to the ear-temporal nerve; 5, 15 - postganglionic parasympathetic fibers; 6 - middle artery of the dura mater; 7 - ear-temporal nerve; 8, 16 - sensitive fibers; 9 - drum string; 11 - nodal branches of the lingual nerve; 12, 19 - switching preganglionic fibers to postganglionic ones; 13 - submandibular nerve; 14 - glandular branches; 17 - lingual nerve; 18 - connecting branch of the ear node to the buccal nerve; 20 - ear node; 21 - nodal branches of the mandibular nerve.

Rice. 241. Facial nerve (diagram).
1 - the bottom of the IV ventricle; 2 - the nucleus of the facial nerve; 3 - styloid opening; 4 - posterior ear muscle; 5 - occipital vein; 6 - the posterior abdomen of the digastric muscle; 7 - stylohyoid muscle; 8 - branches of the facial nerve to facial muscles and platysma; 9 - muscle lowering the corner of the mouth; 10 - chin muscle; 11 - muscle lowering the lower lip; 12 - buccal muscle; 13 - circular muscle of the mouth; 14 - muscle lifting the upper lip; 15 - canine muscle; 16 - zygomatic muscle; 17 - circular muscle of the eye; 18 - muscle wrinkling the eyebrow; 19 - frontal muscle; 20 - drum string; 21 - lingual nerve; 22 - pterygopalatine node; 23 - trigeminal node; 24 - internal carotid artery; 25 - intermediate nerve; 26 - facial nerve; 27 - vestibular cochlear nerve.
the edges of the bridge, between it and the pyramid of the medulla oblongata, and soon outside of the back of the sella turcica enters the cavernous sinus, where it is located along the outer surface of the internal carotid artery. Then it penetrates through the superior orbital fissure into the orbit and follows forward above the oculomotor nerve. In the cavernous sinus, connecting branches from the internal carotid plexus, containing sympathetic nerve fibers, pass to the nerve. Innervates the external rectus muscle of the eye.
VII PAIR - FACIAL NERVES
Facial nerven. facialis, develops in connection with the formations of the second branchial arch (Fig. 241), therefore it innervates all mimic
1 2 3 4 5 6 7 8

Rice. 242. The nerves of the temporal bone canals.
1 - stapes nerve; 2 - drum string; 3 - tympanic plexus; 4 - the connecting branch of the facial nerve with the tympanic plexus; 5 - knee knot; 6 - facial nerve; 7 - intermediate nerve; 8 - vestibular cochlear nerve; 9, 19 - connecting branch from the knee node to the plexus of the middle meningeal artery; 10 - large stony nerve; 11 - carotid-tympanic nerve; 12 - small stony nerve; 13 - internal carotid nerve plexus; 14 - deep stony nerve; 15 - the nerve of the pterygoid canal; 16 - pterygopalatine nerves; 17 - maxillary nerve; 18 - pterygopalatine node; 20 - nerve plexus around the middle meningeal artery; 21 - ear node; 22 - branches of the ear node to the ear-temporal nerve; 23 - connecting branch between the ear unit and the drum string; 24 - chewing nerve; 25 - mandibular nerve; 26 - lingual nerve; 27 - lower alveolar nerve; 28 - ear-temporal nerve; 29 - tympanic nerve; 30 - glossopharyngeal nerve; 31 - the upper node of the vagus nerve; 32 - auricular branch of the vagus nerve; 33 - connecting branch of the facial nerve with the ear branch of the vagus nerve; 34 - branches of the facial nerve to the stylohyoid muscle; 35 - branches of the facial nerve to the posterior abdomen of the digastric muscle; 36 - posterior ear nerve; 37 - mastoid process.
cue muscles. The nerve is mixed, including motor fibers from its efferent cerebral nucleus, as well as sensory and autonomic (taste and secretory) fibers belonging to the intermediate nerve,n. intermedius.
The motor nucleus of the facial nerve,nucleus nervi facialis, is located at the bottom of the IV ventricle, in the lateral region of the reticular formation. The root of the facial nerve leaves the brain together with the root of the intermediate nerve in front of the vestibular cochlear nerve, between the posterior edge of the pons and the olive of the medulla oblongata. Further, the facial and intermediate nerves enter the internal auditory opening and enter the facial canal. In the facial canal, both nerves form a common trunk, making two turns in accordance with the bends of the canal (Fig. 242).
First, the common trunk is located horizontally, heading over the tympanic cavity anteriorly and laterally. Then, according to the bend of the facial canal, the trunk turns at a right angle back, forming a knee, geniculum n. facialis, and a knee knot, ganglion geniculi, belonging to the intermediate nerve. Having passed over the tympanic cavity, the trunk makes a second downward turn, located behind the middle ear cavity. At this site, branches of the intermediate nerve branch off from the common trunk, the facial nerve leaves the canal through the styloid opening and soon enters the parotid salivary gland. The length of the trunk of the extracranial part of the facial nerve ranges from 0.8 to 2.3 cm (usually 1.5 cm), and the thickness - from 0.7 to 1.4 mm; the nerve contains 3500-9500 myelinated nerve fibers, among which thick ones predominate.
In the parotid salivary gland, at a depth of 0.5-1.0 cm from its outer surface, the facial nerve is divided into 2-5 primary branches, which are divided into secondary branches, forming parotid plexus,plexus intraparotideus.
There are two forms of the external structure of the parotid plexus - reticular and trunk. At reticular the trunk of the nerve is short (0.8-1.5 cm), in the thickness of the gland it is divided into many branches that have multiple connections with each other, as a result of which a narrow-looped plexus is formed. There are multiple connections with the branches of the trigeminal nerve. At trunk (form the trunk of the nerve is relatively long (1.5-2.3 cm), it is divided into two branches (upper and lower), which give several secondary branches; there are few connections between the secondary branches, the plexus is wide-looped (Fig. 243).
On its way, the facial nerve gives off branches when passing through the canal, as well as after leaving it. Inside the channel, a number of branches extend from it.
1. Large stony nerve,n. petrosus major, originates near the knee node, leaves the canal of the facial nerve through the cleft of the canal of the greater stony nerve and passes along the groove of the same name to the laceration. Having penetrated through the cartilage to the outer base of the skull, the nerve connects to the deep petrosal nerve, forming nerve of the pterygoid canal,n. canalis pterygoidei, entering the pterygoid canal and reaching the pterygopalatine node.
The nerve contains parasympathetic fibers to the pterygopalatine node, as well as sensory fibers from the cells of the knee node. Part of the sensory fibers in the greater petrosal nerve comes from the pterygopalatine ganglion in the facial nerve.

Rice. 243. Differences in the structure of the facial nerve.
a - network-like structure; b - main structure.
1 - facial nerve; 2 - chewing muscle.
2. Stapes nerven. stapedius, - a thin trunk, branches off in the facial canal at the second turn, penetrates into the tympanic cavity, where it innervates the stapedius muscle.
3. Drum stringchorda tympani, is a continuation of the intermediate nerve, it is separated from the facial nerve in the lower part of the canal above the styloid foramen and enters through the tubule of the tympanic string into the tympanic cavity, where it lies under the mucous membrane between the long leg of the incus and the handle of the hammer. Through the stony-tympanic fissure, the tympanic string comes out to the outer base of the skull and merges with the lingual nerve in the infratemporal fossa.
At the intersection with the inferior alveolar nerve, the tympanic string gives a connecting branch with the ear node. The tympanic string consists of preganglionic parasympathetic fibers to the submandibular node and taste sensory fibers to the anterior two-thirds of the tongue.
4. Connecting branch with tympanic plexus,r. communicans cum plexo tympanico, - thin branch; starts from the knee node or from the large stony nerve, passes through the roof of the tympanic cavity to the tympanic plexus.
Upon exiting the canal, the following branches branch off from the facial nerve.
1. Posterior ear nerven. auricularis posterior, departs from the facial nerve immediately after leaving the styloid foramen, goes back and up along the front surface of the mastoid process, dividing into two branches: ear, r. auricularis, the innervating posterior ear muscle, and the occipital, r. occipitalis, innervating the occipital abdomen of the supracranial muscle.
2. Double-abdominal branch,r. digastricus, arises slightly below the ear nerve and, going down, innervates the posterior abdomen of the digastric muscle and the stylohyoid muscle.
3. Connecting branch with glossopharyngeal nerve,r. communicans cum n. glossopharyngeus, It branches off near the styloid foramen and spreads anteriorly and downward along the stylopharyngeal muscle, connecting with the branches of the glossopharyngeal nerve.
Parotid plexus branches:
1. Temporal branches.rr. temporales, in the amount of 2-4, go up and are divided into 3 groups: the anterior, innervating the upper part of the circular muscle of the eye, and the muscle wrinkling the eyebrow; middle, innervating the frontal muscle; posterior, innervating rudimentary muscles of the auricle.
2. Zygomatic branches,rr. zygomatici, in the amount of 3-4, spread forward and upward to the lower and lateral parts of the circular muscle of the eye and the zygomatic muscle, which it innervates.
3. Cheek branches,rr. buccales, in the amount of 3-5, go horizontally anteriorly along the outer surface of the masseter muscle and supply the muscles with branches in the circumference of the nose and mouth.
4. The marginal branch of the lower jaw,r. marginalis mandibularis, runs along the edge of the lower jaw and innervates the muscles that lower the corner of the mouth and lower lip, the chin muscle and the muscle of laughter.
5. Cervical branch, r. colli, descends to the neck, connects to the transverse nerve of the neck and innervates t. platysma.
Intermediate nerven. intermedius, consists of preganglionic parasympathetic and sensory fibers. Sensitive unipolar cells are located at the knee node. The central processes of the cells ascend as part of the nerve root and end in the nucleus of the solitary pathway. Peripheral processes of sensitive cells go through the tympanic cord and the large petrosal nerve to the mucous membrane of the tongue and soft palate.
Secretory parasympathetic fibers originate in the superior salivary nucleus in the medulla oblongata. The root of the intermediate nerve leaves the brain between the facial and vestibular cochlear nerves, joins the facial nerve and goes into the facial canal. The fibers of the intermediate nerve leave the trunk of the facial, passing into the tympanic string and the large petrosal nerve, reach the submandibular and hyoid nodes and the pterygopalatine node.
QUESTIONS FOR SELF-CONTROL
1. What cranial nerves are mixed in origin?
2. What cranial nerves develop from the forebrain?
3. List the nerves that innervate the muscles of the eyes.
4. Due to which branches is the sensory innervation of the optic nerves carried out? Indicate the areas of this innervation.
5. What branches extend from the optic nerve?
6. What nerves are the upper teeth innervated by? Where do these nerves come from?
7. List the branches of the mandibular nerve.
8. What nerves pass through the drum string?
9. Which branches extend from the facial nerve inside its canal? What do they innervate?
10. What are the branches of the facial nerve in the parotid plexus? What do they innervate?
VIII PAIR - PRE-COLLULAR NERVES
The vestibular cochlear nerven. vestibulocochlearis, - sensitive, consists of two functionally different parts: vestibule and cochlea.
Vestibular nerve n. vestibularis, conducts impulses from the static apparatus of the vestibule and semicircular canals of the labyrinth of the inner ear. Cochlear nerve n. cochlearis, ensures the transmission of sound stimuli from the cochlear spiral organ. Each part of the nerve has its own sensory nodes containing bipolar nerve cells: the vestibule - door knot,ganglion vestibulare, located at the bottom of the internal auditory passage; cochlear part - cochlear node[coiled snail knot], ganglion cochleare, which is in the snail.
The vestibule is elongated, two parts are distinguished in it: the upper, pars superior, and the bottom, pars inferior. The peripheral processes of the cells of the upper part form the following nerves:
1) elliptic saccular nerve,n. utricularis, to the cells of the elliptical sac of the vestibule of the snail;
2) anterior ampullary nerve,n. ampullaris anterior, to the cells of the sensitive strips of the anterior membranous ampulla of the anterior semicircular canal;
3) lateral ampullary nerve,n. ampullaris lateralis, to the lateral membranous ampulla.
From the lower part of the vestibular node, the peripheral processes of the cells are composed of spherical saccular nerve,n. saccularis, to the auditory spot of the sac; posterior ampullary nerve,n. ampullaris posterior, to the posterior membranous ampulla.
The central processes of the cells of the vestibular node form vestibule(upper)root,radix vestibularis (superior), which exits through the internal auditory opening behind the facial and intermediate nerves and enters the brain near the exit of the facial nerve, reaching the 4 vestibular nuclei in the pons: medial, lateral, superior and inferior.
From the cochlear ganglion, the peripheral processes of its bipolar nerve cells go to the sensitive epithelial cells of the
Rice. 244. Glossopharyngeal nerve (diagram).
1 - facial nerve; 2 - tympanic nerve; 3 - the lower node of the glossopharyngeal nerve; 4 - glossopharyngeal nerve; 5 - ear node of the glossopharyngeal nerve; 6 - wing-palatal node; 7 - trigeminal nerve; 8 - small stony nerve; 9 - large stony nerve.
the cochlear organ of the cochlea, forming in aggregate the cochlear part of the nerve. The central processes of the cells of the cochlear node form the cochlear (lower) root, radix cochlearis (inferior), going along with the superior root into the brain to the dorsal and ventral cochlear nuclei.
LANGUAGE NERVES
Glossopharyngeal nerven. glossopharyngeus, - nerve of the third branchial arch, mixed. It innervates the mucous membrane of the posterior third of the tongue, palatine arches, pharynx, tympanic cavity, parotid salivary gland and stylopharyngeal muscle (Fig. 244). The nerve contains 3 types of nerve fibers: 1) sensitive, 2) motor, 3) parasympathetic.
Sensitive fibers - processes of afferent cells top and bottom nodes,ganglia superius et inferius. Peripheral processes follow as part of the nerve to the organs, where they form receptors, the central ones go to the medulla oblongata, to the sensitive nucleus of the solitary pathway, nucleus solitarius.
Motor fibers start from nerve cells in common with the vagus nerve double nucleus, nucleus ambiguus, and pass as part of the nerve to the stylopharyngeal muscle.
Parasympathetic fibers originate in the autonomic parasympathetic lower salivary nucleus, nucleus salivatorius inferior, which is located in the medulla oblongata.
The glossopharyngeal nerve root leaves the medulla oblongata behind the exit site of the vestibular cochlear nerve and, together with the vagus nerve, leaves the skull through the jugular foramen. In this hole, the nerve has its first extension - top node,ganglion superius, and upon exiting the hole - the second expansion - bottom node,ganglion inferius.
Outside the skull, the glossopharyngeal nerve lies first between the internal carotid artery and the internal jugular vein, and then
a log arc bends around the back and outside of the stylopharyngeal muscle and approaches from the inside of the hyoid-lingual muscle to the root of the tongue, dividing into terminal branches.
Branches of the glossopharyngeal nerve:
1. Tympanic nerven. tympanicus, branches off from the lower node and passes through the tympanic tubule into the tympanic cavity, where it forms, together with the carotid-tympanic nerves tympanic plexus,plexus tympanicus. The tympanic plexus innervates the mucous membrane of the tympanic cavity and auditory tube. The tympanic nerve leaves the tympanic cavity through its superior wall as small stony nerve,n. petrosus minor, and goes to the ear node. The preganglionic parasympathetic secretory fibers, which are part of the small petrosal nerve, are interrupted in the ear node, and the postganglionic secretory fibers enter the auricular-temporal nerve and reach the parotid salivary gland.
2. A branch of the stylopharyngeal muscle,r. musculi stylopharyngei, goes to the muscle of the same name and the mucous membrane of the pharynx.
3. Sinus branchr. sinus carotici, sensitive, branches in the sleepy glomus.
4. Amygdala branches,rr. tonsillares, are directed to the mucous membrane of the palatine tonsil and arches.
5. Pharyngeal branchesrr. pharyngei, in the amount of 3-4, approach the pharynx and, together with the pharyngeal branches of the vagus nerve and the sympathetic trunk, form on the outer surface of the pharynx pharyngeal plexus,plexus pharyngeus. Branches extend from it to the muscles of the pharynx and mucous membrane, which in turn form intramural nerve plexuses.
6. Lingual branches,rr. linguales, - terminal branches of the glossopharyngeal nerve: contain sensitive taste fibers to the mucous membrane of the posterior third of the tongue.
X PAIR - WALKING NERVES
Nervus vagus,n. vagus, mixed, develops from 4-5th gill arcs, spreads widely, which is why it got its name. It innervates the respiratory organs, organs of the digestive system (up to the sigmoid colon), the thyroid and parathyroid glands, adrenal glands, kidneys, participates in the innervation of the heart and blood vessels.
The vagus nerve contains sensory, motor and autonomic parasympathetic and sympathetic fibers, as well as intra-trunk small nerve nodes (Fig. 245).

Rice. 245. Vagus and accessory nerves (diagram).
1 - connecting branch of the vagus nerve with the facial; 2 - glossopharyngeal nerve; 3 - accessory nerve; 4 - the connecting branch of the vagus nerve with the hypoglossal; 5 - connecting branch of the vagus nerve with a sympathetic trunk; 6 - language; 7 - the hyoid bone; 8 - larynx; 9 - trachea; 10 - the right recurrent laryngeal nerve;
11 - left recurrent laryngeal nerve; 12 - left vagus nerve; 13 - aortic arch; 14 - left lung; 15 - heart; 16 - diaphragm; 17 - stomach; 18 - liver; 19 - the right lunate node of the celiac plexus; 20 - a nerve node on the ascending part of the aorta; 21 - right lung; 22 - esophagus; 23 - branches of the right recurrent laryngeal nerve; 24 - superior laryngeal nerve; 25 - trapezius muscle; 26 - sternocleidomastoid muscle; 27 - accessory nerve; 28 - nuclei of the vagus and accessory nerves; 29 - the nucleus of the vagus nerve; 30 - facial nerve.
Sensory nerve fibers of the vagus nerve originate from afferent pseudo-unipolar nerve cells, the accumulations of which form 2 sensory nerve nodes: the upper, ganglion superius, located in the jugular foramen, and lower, ganglion inferius, lying on the exit from the hole. The central processes of the cells go to the medulla oblongata to the sensitive nucleus - the core of a single path,nucleus solitarius, and peripheral - as part of the nerve to the vessels, heart and internal organs, where they end with receptor apparatus.
Motor fibers for the muscles of the soft palate, pharynx and larynx originate from the upper motor cells double core.
Parasympathetic fibers come from the vegetative dorsal nucleus,nucleus dorsalis n. vagi, and are distributed as part of the nerve to the heart muscle, muscle tissue of the vascular membranes and internal organs... The impulses traveling along the parasympathetic fibers reduce the heart rate, dilate blood vessels, narrow the bronchi, and increase the peristalsis of the tubular organs of the gastrointestinal tract.
Autonomic postganglionic sympathetic fibers enter the vagus nerve along its connecting branches with the sympathetic trunk from the cells of the sympathetic nodes and spread along the branches of the vagus nerve to the heart, blood vessels and internal organs.
As noted, the glossopharyngeal and accessory nerves are separated from the vagus nerve during development, so the vagus nerve maintains connections with these nerves, as well as with the hypoglossal nerve and the sympathetic trunk through the connecting branches.
The vagus nerve leaves the medulla oblongata behind the olive in numerous roots, merging into a common trunk, which exits the skull through the jugular foramen. Further, the vagus nerve goes downward as part of the cervical neurovascular bundle, between the internal jugular vein and the internal carotid artery, and below the level of the upper edge of the thyroid cartilage - between the same vein and the common carotid artery. Through the superior aperture of the chest, the vagus nerve penetrates between the subclavian vein and the artery on the right and in front of the aortic arch on the left into the posterior mediastinum. Here it forms in front of the esophagus (left nerve) and behind it (right nerve) by branching and connections between branches esophageal plexus,plexus esophageus, which, near the esophageal opening of the diaphragm, forms 2 vagus trunks: anterior, truncus vagalis anterior, and rear, truncus vagalis posterior, corresponding
left and right vagus nerves. Both trunks leave the chest cavity through the esophageal opening, give branches to the stomach and end in a number of terminal branches in celiac plexus. From the plexus, the fibers of the vagus nerve spread along the branches of this plexus. Throughout the vagus nerve branches depart from it (Fig. 246).
Branches of the head section of the vagus nerve:
1. Meningeal branchr. meningeus, starts from the superior node and goes through the jugular foramen, reaches the dura mater of the posterior fossa of the skull.
2. Ear branch,r. auricularis, goes from the upper node along the anterolateral surface of the bulb of the jugular vein to the entrance to the mastoid canal and then along it to the back wall of the external auditory canal and part of the skin of the auricle. On its way, it forms connecting branches with the glossopharyngeal and facial nerves.
Branches cervical vagus nerve:
1. Pharyngeal branchesrr. pharyngei, originate from the bottom node or just below it. Thin branches are taken from the upper cervical node of the sympathetic trunk and between the external and internal carotid arteries they penetrate to the lateral wall of the pharynx, on which, together with the pharyngeal branches of the glossopharyngeal nerve and the sympathetic trunk, they form the pharyngeal plexus.
2. Superior laryngeal nerven. laryngeus superior, branches off from the lower node and descends down and forward along the lateral wall of the pharynx inwards from the internal carotid artery. At the large horn, the hyoid bone is divided into two branches: the outer, r. externus, and internal, r. internus. The outer branch connects to the branches from the upper cervical node of the sympathetic trunk and goes along the posterior edge of the thyroid cartilage to the cricothyroid muscle and the lower constrictor of the pharynx, and also irregularly gives branches to the arytenoid and lateral cricoid muscles. In addition, branches branch off from it to the mucous membrane of the pharynx and the thyroid gland. The inner branch is thicker, more sensitive, pierces the thyroid-hyoid membrane and branches in the mucous membrane of the larynx above the glottis, as well as in the mucous membrane of the epiglottis and the anterior wall of the nasal part of the pharynx. Forms a connecting branch with the lower laryngeal nerve.
3. Upper cervical cordial branches,rr. cardiaci cervicales superiores, - branches varying in thickness and level, usually thin, originate between the superior and recurrent laryngeal nerves and go down to the cervicothoracic nerve plexus.

Rice. 246. Vagus and glossopharyngeal nerves and sympathetic trunk. 1 - lower cervical cardiac branches of the vagus nerve; 2 - recurrent laryngeal nerve; 3 - upper cervical cordial branches; 4 - pharyngeal plexus; 5 - hypoglossal nerve; 6 - the superior laryngeal nerve; 7 - lingual nerve; 8 - pharyngeal branches of the vagus nerve; 9 - glossopharyngeal nerve; 10, 11 - branches of the accessory nerve; 12, 15, 17, 19 - 2nd, 3rd, 4th and 5th cervical spinal nerves; 13 - upper cervical node of the sympathetic trunk; 14, 16 - vagus nerve; 18 - phrenic nerve; 20 - middle cervical node of the sympathetic trunk; 21 - brachial plexus; 22 - lower cervical node of the sympathetic trunk; 23, 24, 26, 28 - 2nd, 3rd, 4th and 5th chest nodes of the sympathetic trunk; 25 - recurrent laryngeal nerve; 27 - pulmonary plexus.
4. Lower cervical cordial branches,rr. cardiaci cervicales inferiores, depart from the laryngeal recurrent nerve and from the trunk of the vagus nerve; participate in the formation of the cervicothoracic nerve plexus.
Branches of the thoracic vagus nerve:
1. Recurrent laryngeal nerven. laryngus recurrens, departs from the vagus nerve when it enters the chest cavity. The right recurrent laryngeal nerve goes around the subclavian artery from below and behind, and the left - the aortic arch. Both nerves rise in the groove between the esophagus and trachea, giving branches to these organs. The final branch is lower laryngeal nerve,n. laryngeus inferior, approaches the larynx and innervates all the muscles of the larynx, with the exception of the cricothyroid, and the mucous membrane of the larynx below vocal cords.
Branches extend from the recurrent laryngeal nerve to the trachea, esophagus, thyroid and parathyroid glands.
2. Thoracic heart branches,rr. cardiaci thoracici, start from the vagus and left laryngeal recurrent nerves; participate in the formation of the cervicothoracic plexus.
3. Tracheal branches go to the thoracic trachea.
4. Bronchial branches are sent to the bronchi.
5. Esophageal branches fit to the thoracic esophagus.
6. Pericardial branches innervate the pericardium.
Within the cavities of the neck and chest, the branches of the vagus, recurrent and sympathetic trunks form the cervicothoracic nerve plexus, in which organ plexuses are distinguished: thyroid, tracheal, esophageal, pulmonary, cardiac.
The branches of the vagus trunks (abdominal part):
1. Anterior gastric branches start from the anterior trunk and form the anterior gastric plexus on the anterior surface of the stomach.
2. Posterior gastric branches depart from the posterior trunk and form the posterior gastric plexus.
3. Celiac branches depart mainly from the posterior trunk and take part in the formation of the celiac plexus.
4. Hepatic branches are part of the hepatic plexus.
5. Renal branches form the renal plexus.
XI PAIR - SUPPLEMENTARY NERVE
Accessory nerven. accessorius, mainly motor, separated during development from the vagus nerve. Begins
in two parts - the vagus and the spinal cord - from the corresponding motor nuclei in the medulla oblongata and spinal cord. Afferent fibers enter the trunk through the spinal cord from the cells of the sensory nodes.
The wandering part comes out cranial rootsradices craniales, from the medulla oblongata below the exit of the vagus nerve, the spinal part is formed from spinal roots,radices spinales, leaving spinal cord between the back and front roots. The spinal part of the nerve rises to the foramen magnum, enters through it into the cranial cavity, where it connects with the vagus part and forms a common nerve trunk.
In the cranial cavity, the accessory nerve is divided into two branches: internal and outdoor.
1. Inner branch,r. internus, approaches the vagus nerve. Through this branch, motor nerve fibers are included in the vagus nerve, which leave it through the laryngeal nerves. It can be assumed that sensory fibers also pass into the vagus and further into the laryngeal nerve.
2. Outer branch,r. externus, leaves the cranial cavity through the jugular opening to the neck and goes first behind the posterior abdomen of the digastric muscle, and then from the inside of the sternocleidomastoid muscle. Perforating the last, the outer branch goes down and ends in the trapezius muscle. Connective connections are formed between the accessory and cervical nerves. It innervates the thoracic-clavicular-mastoid and trapezius muscles.
XII PAIR - SUBLINGUAL NERVE
Hyoid nerven. hypoglossus, predominantly motor, formed as a result of the fusion of several primary spinal segmental nerves that innervate the hypoglossal muscles. Other types of fibers also pass through the hypoglossal nerve. Sensory nerve fibers come from the cells of the inferior node of the vagus nerve and, possibly, from the cells of the spinal nodes along the connecting branches between the hypoglossal, vagus and cervical nerves. Sympathetic fibers enter the hypoglossal nerve along its connecting branch with the superior node of the sympathetic trunk (Fig. 247).
The nerve fibers that make up the hypoglossal nerve depart from its cells motor nucleus, located in the medulla oblongata. The nerve comes out of it between the pyramid and the olive with several roots. The formed trunk of the nerve passes through the ascent

Rice. 247. Hyoid nerve (diagram).
1 - diamond-shaped fossa; 2 - the canal of the hypoglossal nerve; 3 - connecting branches of the hypoglossal nerve with the upper cervical node of the sympathetic trunk and the lower node of the vagus nerve; 4 - the hypoglossal nerve; 5, 6 - branches to the muscles of the tongue; 7 - branches to the sublingual muscle; 8 - the hyoid bone; 9 - a branch to the sternohyoid muscle; 10 - branches to the sternohyoid muscle; 11 - branches to the sterno-thyroid muscle; 12 - a branch to the scapular-hyoid muscle; 13 - internal jugular vein; 14 - lower root of the hyoid loop; 15 - the upper root of the hyoid loop; 16 - internal jugular vein; 17 - internal carotid artery; 18 - 1st and 3rd cervical spinal nerves; 19 - the nucleus of the hypoglossal nerve.
the lingual canal on the neck, where it is located first between the external (outside) and internal carotid arteries, and then descends under the posterior abdomen of the digastric muscle in the form of an open upward arc along the lateral surface of the hyoid-lingual muscle, making up the upper side of the Pirogov triangle; branches into terminal lingual branches,rr. linguales, innervating muscles of the tongue.
From the middle of the arc of the nerve down along the common carotid artery goes upper spine of the neck loop,radix superior, which connects with her lower spine,radix inferior, from the cervical plexus, resulting in the formation neck loop,ansa cervicalis. Several branches extend from the neck loop to the neck muscles located below the hyoid bone.
The position of the hypoglossal nerve on the neck can vary. In people with a long neck, the arch formed by the nerve lies relatively low, while in people with a short neck, it is high. It is important to take this into account during operations on the nerve (Table 15).
Table 15. Areas of innervation, fiber composition and names of the nuclei of the cranial nerves
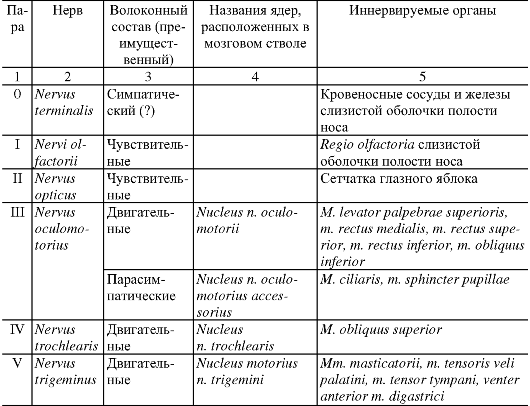
Continuation of table. 15

The end of the table. 15

QUESTIONS FOR SELF-CONTROL
1. What nerves extend from the vestibule node?
2. List the branches of the glossopharyngeal nerve.
3. What branches extend from the head and cervical parts of the vagus nerve? What do they innervate?
4. List the branches of the thoracic and abdominal vagus nerve. What do they innervate?
5. What do the accessory and hypoglossal nerves innervate?
The development of cranial nerves is closely related: 1) with the development of the central nervous system, its differentiation from the primary neural tube, 2) with the development of muscles and skin (somite derivatives), 3) with the primary anlages of internal organs and the cardiovascular system.
The factors that determine the complexity of the development of the cranial nerves are: the development of the sense organs and visceral arches and the reduction of the cephalic somites.
Motor nerves arise by the growth of nerve fibers from the motor nuclei in the developing brain into the muscle buds.
Sensory nerves arise by the growth of processes of nerve cells located in the nerve nodes. Some processes of these cells grow into the brain, others into skin or mucous membranes. The sensory nodes of the cranial nerves develop in the same way as the spinal nodes, through the migration of nerve cells from the ganglionic ridges.
The first and second pairs of cranial nerves are outgrowths of the brain, they are the brain itself, brought out to the periphery: the first pair is the outgrowth of the olfactory (terminal) brain, the second pair is the intermediate one. By their structure and origin, they occupy a special position among the cranial nerves, since they do not have nuclei in the brain and, being sensory nerves, do not have sensory nodes. So these nerves are the brain itself, they don't need nuclei.
The third, fourth, sixth pairs in their development are associated with the midbrain (the nucleus of the sixth pair is later shifted to the bridge) and three head (preauricular) myotomes, from which the muscles of the eyeball develop (Fig. 1). The first preauricular myotome corresponds to the third nerve, the second to the fourth nerve, and the third to the sixth nerve.
The fifth, seventh, ninth, tenth, eleventh pairs of cranial nerves in their development are associated with the rhomboid brain and visceral arches (Fig. 1). These are nerves of branchial origin.
Rice. 1.: III-XII - cranial nerves; 1-5 - visceral arches; 6 - preauricular myotomes; 7 - behind the ear myotomes.
First visceral arch - mandibular... The development of the V pair of cranial nerves is associated with it. On its basis, the chewing apparatus develops: the chewing muscles, the muscles of the bottom of the mouth.
The second visceral arch is hyoid... The development of the seventh pair is associated with it, from which the eighth nerve is further separated. On the basis of this arch, the hyoid bone and facial muscles are formed.
Third visceral arch- the ninth nerve corresponds to it, the stylopharyngeal muscle develops from the arch.
Fourth visceral arch- the tenth nerve corresponds to it, the muscles of the larynx, the muscles of the pharynx, palate develop.
Fifth visceral arch- the eleventh nerve corresponds to it, the sternocleidomastoid and trapezius muscles develop.
The twelfth pair of cranial nerves develops by fusion of the superior cervical spinal nerves and is associated with the myotomes behind the ear, from which the muscles of the tongue are formed.
The structure of the cranial nerves, in principle, does not differ from the structure of the spinal nerves, although there are a number of features: 1) none of the cranial nerves corresponds to the complete spinal nerve, does not have two roots that leave the brain separately and then join; 2) the cranial nerves, like the spinal nerves, contain motor, sensory and autonomic fibers, but not all nerves are mixed.
Consider a plan of the structure of the cranial nerve containing only sensory fibers corresponding to the posterior root of the spinal nerve. Such a nerve necessarily has a node with sensory pseudo-unipolar cells outside the brain and sensory nuclei in the brain corresponding to the sensory nuclei of the dorsal horns of the spinal cord.
The cranial nerve can contain only motor or motor and autonomic fibers, corresponding to the anterior root of the spinal nerve. In this case, the nerve has motor and autonomic nuclei in the brain, as does the spinal nerve. However, sympathetic autonomic fibers pass through the spinal nerve, and parasympathetic fibers pass through the cranial nerves. And finally, there are the cranial nerves, which contain sensory, motor and parasympathetic fibers.
First pair - nervi olfactorii
The olfactory nerves (there are about 20 of them) are sensory nerves that do not have anatomically shaped sensory nuclei and nodes. They consist of processes of sensitive cells of the olfactory epithelium - filia olfactoria. The low strength of the thin olfactory nerves and their fixation in the holes of the lamina cribrosa by the dura mater causes ruptures or pressing in trauma, tumors and brain edema, etc., which leads to a decrease or loss of smell.
The sense of smell is tested using a set of scent essences separately for each side.
The second pair is nervus opticus
The optic nerve is part of the brain itself, so it doesn't need a nucleus. As a nerve of special sensitivity, it does not have an anatomically shaped node. It is formed from the processes of multipolar retinal cells. Each optic nerve is made up of approximately a million fibers that send signals from the retina to the brain. Along the course of the nerve, 4 parts are distinguished: 1) intraocular, pars intraocularis, 2) orbital, pars orbitalis, 3) canal, pars canalis and 4) intracranial, pars intracranialis. The second, third and fourth parts of the nerve are surrounded by the membranes of the brain and cerebrospinal fluid.
Ophthalmologists have visual acuity charts and visual field devices.
Complete damage to the optic nerve leads to blindness, partial - to the loss of certain areas of the visual field - the appearance of a slope.
Third, fourth, sixth pairs - n. oculomotorius, n. trochlearis, n. abducens
The oculomotor nerve contains motor and autonomic fibers. It is known that the motor nucleus consists of 5 groups of cells. Fibers from individual groups of the nucleus innervate certain muscles of the eyeball: the upper rectus, the muscle that lifts the upper eyelid, the lower oblique, medial and lower rectus muscles. Parasympathetic nucleus, n. accessorius nervi oculomotorii, or Yakubovich's nucleus, innervates the muscle that narrows the pupil, m. sphincter pupillae, and Pearl's nucleus is n. caudatus centralis, innervates the ciliary muscle, m. ciliaris participating in accommodation.
The block and abducens nerves are purely motor. The block innervates the superior oblique muscle, and the abductor innervates the external rectus muscle of the eyeball (Fig. 2, 3). So, three nerves regulate the voluntary movement of the eyeball, and the oculomotor nerve also controls the degree of curvature of the lens during focusing and the constriction of the pupil in bright light.

Rice. 2..

Rice. 3. (according to S.Yu. Stebelsky).
The nuclei of the third, fourth, sixth nerves have bilateral cortical innervation, that is, tr. corticonuclearis goes on its own and the opposite side, therefore, the function of the nerves with unilateral damage to the nuclei does not suffer.
All the nerves leaving the brain, firstly, are in the subarachnoid space, then they pierce the dura mater; secondly, they pass through the superior orbital fissure; thirdly, they pass through the cavernous sinus. Therefore, peripheral lesions of the nerves are observed 1) with meningitis and arachnoiditis; 2) with injuries and tumors in the superior orbital fissure and 3) with inflammation or thrombosis of the cavernous sinus.
Based on the knowledge of the topography of the nerves and their nuclei, the work of the muscles they innervate, a doctor of any profile must make a topical diagnosis and promptly refer the patient to a neurologist, since a brain tumor develops rapidly and is always malignant along the course. For example, in a patient, the left eye turns to the right, therefore, the left third nerve is normal, and when moving to the left, it stops, therefore, the left sixth nerve does not work. The pathological process is located not in the orbit, but further, at the exit of the left sixth nerve from the brain, at the level of the lower edge of the bridge, where these nerves are pulled apart (Fig. 4).

Rice. 4.: I-XII - cranial nerves; 1 - eyeball; 2 - the temporal lobe of the cerebral hemisphere; 3 - the leg of the brain; 4 - bridge; 5 - cerebellum; 6 - pyramid of the medulla oblongata; 7 - spinal cord.
The fifth nerve - n. trigeminus
The trigeminal nerve contains motor and sensory fibers. Does not have any vegetative. The sensory node of the trigeminal nerve lies in the region of the trigeminal depression on the pyramid of the temporal bone and is called the Gasser node.
The trigeminal nerve leaves the bridge at the border with the middle cerebellar pedicle by two roots - sensory and motor. The peripheral processes of the pseudo-unipolar cells of the trigeminal node form three branches (Fig. 5). Motor fibers are attached only to the third branch.

Rice. 5. Diagram of connections of parasympathetic fibers of the third, seventh and ninth cranial nerves with parasympathetic nodes and branches of the fifth cranial nerve: 1 - n. ophthalmicus; 2 - n. maxillaris; 3 - n. mandibularis; 4 - n. frontalis; 5 - n. lacrimalis; 6 - n. supraorbitalis; 7 - n. nasociliaris; 8 - gangl. ciliare; 9 - n. zygomaticus; 10; 11 - n. infraorbitalis; 12 - nn. alveolares superiores; 13 - n. buccalis; 14 - gangl. pterygopalatinum; 15 - n. lingualis; 16 - n. al-veolaris inferior; 17 - n. mentalis; 18 - gangl. oticum; 19 - n. auriculotemporalis; 20 - n. petrosus major; 21 - gangl. sub- mandibulare; 22 - n. petrosus minor; 23 - n. chorda tympani; 24 - radix motoria.
The first branch is optic nerve penetrates into the orbit through the superior orbital fissure, the second - maxillary nerve goes through the round hole, and the third branch - mandibular nerve- through the oval opening of the skull.
The trigeminal nerve innervates the masseter muscles and other muscles that develop from the first visceral arch. Provides sensitive innervation to the skin of the face, conjunctiva of the eye, mucous membranes of the nasal and oral cavities and teeth. From the sensitive nuclei of the trigeminal nerve, the trigeminal loop begins, lemniscus trigeminalis, which ends in the optic tubercle, then the processes of the nuclei of the optic tubercle pass through the inner capsule to g. postcentralis.
In the course of the branches of the trigeminal nerve, the parasympathetic ganglia are located, in which the parasympathetic fibers belonging to the third, seventh and ninth nerves switch.
Postganglionic parasympathetic fibers go further to the organ as part of the branches of the fifth nerve, using its branches as "rails" (Fig. 5, 6, 10).

Rice. 6.: 1 - trigeminal node; 2 - mandibular nerve; 3 - large stony nerve; 4 - facial nerve; 5 - ear-temporal nerve; 6 - lingual nerve; 7 - buccal nerve; 8 - lower alveolar nerve; 9- chin nerve; 10 - the nerve of the pterygoid canal; 11 - pterygopalatine node; 12 - nodal branches; 13 - upper alveolar nerves; 14 - infraorbital nerve; 15 - zygomatic nerve; 16 - connecting branch; 17 - the lacrimal nerve; 18 - supraorbital nerve; 19 - frontal nerve; 20 - short ciliary nerves; 21 - ciliary node; 22 - nasal nerve; 23 - optic nerve; 24 - maxillary nerve.
With unilateral damage to the motor nucleus of the trigeminal nerve, the chewing function does not suffer, since the nucleus receives tr fibers. corticonuclearis from two hemispheres.
When the trigeminal nerve and its motor branches are damaged, spasm (trismus) or paralysis of the masticatory muscles and their atrophy is observed, and when sensitive branches are damaged, burning pains in the places where the cutaneous branches exit from the skull. Painful pressure on these points (method of examining the fifth nerve). Each of the three branches of the trigeminal nerve innervates a third of the facial skin (Fig. 7) - these are three zones of peripheral innervation of the facial skin by the branches of the fifth nerve.

Rice. 7.: 1 - optic nerve; 2 - the maxillary nerve; 3 - mandibular nerve.
On the other hand, the fibers of the fifth nerve that innervate the skin of the face carry irritations from certain areas of the skin to certain parts of the nucleus, n. spinalis nervi trigemini (Fig. 8). The fibers extending from the medial parts of the face end in the upper parts of this nucleus, regardless of which of the three branches they pass through. The fibers extending from the lateral areas of the facial skin end in the lower parts of the nucleus. Consequently, segmentation is noted in the innervation of the facial skin. This segmentation is manifested in the defeat of n. spinalis nervi trigemini. In these cases, the areas of sensitivity disorders on the face do not coincide with the areas of distribution in the skin of the branches of the fifth nerve, but are segmental, "bulbous" in nature - in the form of arcuate stripes, five Zelder zones.

Rice. eight. .
The seventh nerve - n. facialis
The facial nerve is a mixed nerve that contains motor, sensory and parasympathetic fibers. The facial nerve carries out the motor innervation of the facial muscles and muscles derived from the second visceral arch.
As part of the facial nerve, the old anatomists described the intermediate nerve, so as not to call it the thirteenth nerve in order to avoid trouble. The facial nerve and the intermediate nerve have the same development, they are intertwined, however, these are different nerves. The facial nerve, through the fibers of the intermediate nerve, is the taste nerve for the anterior two-thirds of the tongue and the parasympathetic secretory nerve for all glands of the face except the parotid.
The facial nerve leaves the brain at the pontine-cerebellar angle and then passes through the canal of the facial nerve of the temporal bone. The motor branches of the facial nerve to the facial muscles pass through the thickness of the parotid gland (Fig. 9).

Rice. 9. Superficial nerves of the head and neck: 1 - rami temporalis VII p.: 2 - n. supraorbitalis of the fifth nerve; 3 - rr. zygomatici VII n .; 4 - n infraorbitalis of the fifth nerve; 5 - rr. buccales VII n .; 6 - n. facialis; 7 - n. mentalis; 8 - r. marginalis mandibularis VII n .; 9 - r. colli VII n .; 10 - n. transversus colli; 11 - nn. supraclaviculares; 12 - n. accessorius; 13 - n. auricularis magnus; 14 - n. occipitalis minor; 15 - n. occipitalis major; 16 - n. auriculotemporalis.
Research methods of the facial nerve. On examination, the asymmetry of the skin folds, eye slits, and the level of standing of the corners of the mouth are revealed. Mimic muscles are examined during motor load, asking the examinee to close both eyes, raise eyebrows, show teeth, fold lips with a tube and whistle, close lips and puff out cheeks. The taste in the front two-thirds of the tongue is usually tested for sweet and sour by dripping liquid solutions onto the tongue.
If the motor function of the nerve is impaired, paralysis of the facial muscles is observed. With a unilateral lesion, asymmetry of the face occurs due to the traction of the muscles of the healthy side. In addition, the eyelids do not close, the palpebral fissure remains open due to damage to the circular muscle of the eye. The defeat of the circular muscle of the mouth and buccal muscle leads to difficulty in speaking and eating.
The pathological process in the bridge affects not only the nuclei of the seventh nerve, but also the nearby nucleus of the sixth, adding the corresponding symptoms of damage to neighboring formations.
The eighth nerve - n. vestibulocochlearis
The vestibular cochlear nerve is sensitive, conducts auditory impulses from the spiral organ and information about the position of the body according to the orientation of the head and movement of the body in space.
The cochlear (spiral) node is located in the spiral canal of the cochlea, the vestibular node - in the internal auditory canal. Coming out of the internal auditory canal, the eighth nerve enters the bridge in the region of the cerebellar pontine angle.
Damage to the vestibular part of the seventh nerve is manifested by dizziness, impaired stability of the body at rest, impaired coordination of movements, and damage to the auditory part is manifested by a decrease, distortion of hearing or deafness. Normally, a person should hear a whisper in one ear at a distance of 4-6 meters.
The vestibular apparatus is checked in a special chair. After 10 revolutions on the chair in one direction and 10 in the other, the subject should walk 10 meters straight.
Ninth nerve (n. Glossopharyngeus)
The glossopharyngeal nerve is mixed in function, has motor, sensory and parasympathetic fibers. The glossopharyngeal nerve leaves the medulla oblongata from the dorsolateral groove, and from the cranial cavity through the jugular foramen, within which its sensory nodes are located. Then the nerve is located between the internal carotid artery and the internal jugular vein, passes to the stylopharyngeal muscle and splits into the terminal lingual branches.
The ninth nerve is the sensory nerve for the posterior third of the tongue, soft palate, middle ear and pharynx, the motor nerve for the stylopharyngeal muscle, and the secretory nerve for the parotid gland.
The tenth nerve - n. vagus
The vagus nerve, also a mixed nerve. The tenth nerve innervates the muscles of the pharynx, soft palate, larynx, their mucous membrane, all organs of the chest and abdominal cavities up to the sigmoid colon.
The vagus nerve leaves the dorsolateral groove of the medulla oblongata, leaves the skull through the jugular foramen. In the neck region, the nerve is part of the neurovascular bundle along with the common carotid artery and the internal jugular vein within the carotid triangle. Through the upper aperture it enters the chest cavity, located first in the upper mediastinum, and then in the posterior one (Fig. 10-12). It passes into the abdominal cavity through the esophageal opening, with the left vagus nerve forming the anterior plexus of the esophagus and stomach, and the right one - the posterior one. The nerve innervation zone extends to the sigmoid colon.

Rice. 10.: I - n. opticus; 2 - n. oculomotorius; 3 - n. ophthalmicus; 4 - n. maxillaries; 5 - n. mandibularis; 6 - n. occipitalis major; 7 - radix inferior ansa cervicalis; 8 - ramus superior ansa cervicalis XII n .; 9 - n. auricularis magnus; 10 - n. accessorius; II - n. vagus; 12 - rami muscularis; 13 - nn. supraclaviculares; 14 - n. phrenicus; 15 - n. frontalis; 16 - n. lacrimalis; 17 - n. infraorbitalis; 18 - rami alveolares superiores posteriors; 19 - ramus alveolaris superior medius; 20 - n. lingualis; 21 - n. alveolaris inferior; 22 - n. hypoglossus.

Rice. 11.: 1 - m. styloglossus; 2 - truncus sympathicus; 3 - n. vagus; 4 - n. cardiacus cervicalis superior; 5 - r. cardiacus cervicalis superior; 6 - n. laryngeus recurrens; 7 - n. cardiacus cervicalis inferior; 8 - m. scalenus anterior; 9 - n. hypoglossus; 10 - gangl. cervicale superior; 11 - n. vagus.

Rice. 12.: I - accessory nerve; 2 - the lower node of the vagus nerve; 3 - internal carotid artery; 4 - glossopharyngeal nerve; 5 - pharyngeal branch of the vagus nerve; 6 - common carotid artery; 7 - the right vagus nerve; 8 - recurrent laryngeal nerve; 9 - brachiocephalic trunk; 10 - the right main bronchus; II - left right pulmonary vein; 12 - pulmonary trunk; 13 - esophageal plexus; 14 - left vagus nerve; 15 - the left lobe of the liver; 16 - celiac trunk; 17 - the abdominal part of the aorta; 18 - duodenum.
Isolated lesions of the ninth or tenth nerve are rare. When two nerves are involved in the process, swallowing disorders are observed (food enters the larynx or pours out into the nasal cavity), the voice acquires a nasal tone. Complete loss of vagus nerve function is incompatible with life.
Eleventh nerve - n. accessorius
The accessory nerve is a motor nerve. Correspondingly, the two motor nuclei of the nerve have cranial and spinal roots. The spinal root rises through the foramen magnum, connects to the cranial root, and together they leave the skull through the jugular foramen.
The accessory nerve innervates the muscles: sternocleidomastoid and trapezius. When the nerve is damaged, paralysis and atrophy of these muscles develop.
With a bilateral lesion, the head hangs down on the chest.
The twelfth nerve - n. hypoglossus
The hypoglossal nerve is also a motor nerve. From the medulla oblongata it leaves the roots through the ventro-lateral groove, from the cranial cavity through the canalis hypoglossalis. Descends between the internal carotid artery and the internal jugular vein into the submandibular triangle (Fig. 10, 11).
Here, the nerve takes the superior root from the anterior branches of the 1st and 2nd cervical spinal nerves, which goes to the formation of a deep cervical loop. For 2 cm, this root follows along with the hypoglossal nerve, using its sheath as a cable. After the superior root of the deep cervical loop emerges, the hypoglossal nerve forms an arc and enters the thickness of the tongue, innervating its muscles.
When a nerve is damaged, paralysis of the muscles of the tongue of the opposite side occurs. When protruding the tongue, its deviation towards the lesion is noticeable, since healthy muscles push the tongue more strongly.
Sources and Literature
- A. V. Kondrashev, O. A. Kaplunov. Anatomy of the nervous system. M., 2010.
text_fields
text_fields
arrow_upward
In mammals, including humans, 12 pairs of cranial (cranial) nerves, in fish and amphibians - 10, since their XI and XII pairs of nerves depart from the spinal cord.
The cranial nerves include afferent (sensory) and efferent (motor) fibers of the peripheral nervous system. Sensory nerve fibers begin with terminal receptor endings that perceive changes that occur in the external or internal environment of the body. These receptor endings can enter the sense organs (organs of hearing, balance, sight, taste, smell), or, as, for example, skin receptors, form encapsulated and non-encapsulated endings that are sensitive to tactile, temperature, and other stimuli. Through sensitive fibers, impulses enter the central nervous system. Similar to the spinal nerves, in the cranial nerves, sensory neurons lie outside the CNS in the ganglia. The dendrites of these neurons go to the periphery, and the axons follow to the brain, mainly to the brain stem, and reach the corresponding nuclei.
Motor fibers innervate the skeletal muscles. They form neuromuscular synapses on muscle fibers. Depending on which fibers predominate in the nerve, it is called sensory (sensory) or motor (motor). If a nerve contains both types of fibers, it is called a mixed nerve. In addition to these two types of fibers, fibers of the autonomic nervous system, its parasympathetic division, are present in some cranial nerves.
I pair - olfactory nerves and II pair - optic nerve
text_fields
text_fields
arrow_upward
I pair- olfactory nerves (n. Olfactorii) and II pair- the optic nerve (n. Opticus) occupy a special position: they are referred to the conduction section of the analyzers and are described together with the corresponding sense organs. They develop as outgrowths of the anterior bladder of the brain and are pathways (tracts), not typical nerves.
III – XII pairs of cranial nerves
text_fields
text_fields
arrow_upward
III – XII cranial nerves differ from spinal nerves due to the fact that the conditions for the development of the head and brain are different from the conditions for the development of the trunk and spinal cord. Due to the reduction of myotomes, few neurotomes remain in the head region. In this case, the cranial nerves innervating myotomes are homologous to the incomplete spinal nerve, which is composed of the ventral (motor) and dorsal (sensory) roots. Each somatic cranial nerve includes fibers homologous to one of these two roots. Due to the fact that derivatives of the branchial apparatus take part in the formation of the head, the cranial nerves, in addition, also include fibers that innervate the formations that develop from the muscles of the visceral arches.
III, IV, VI and XII pairs of cranial nerves
text_fields
text_fields
arrow_upward
III, IV, VI and XII pairs of cranial nerves - oculomotor, block, abducens and hypoglossal - are motor and correspond to the ventral, or anterior, roots of the spinal nerves. However, in addition to motor fibers, they also contain afferent ones, along which proprioceptive impulses from the musculoskeletal system rise. Nerves III, IV and VI branch out in the muscles of the eyeball, originating from the three anterior (preauricular) myotomes, and XII in the muscles of the tongue, developing from the occipital myotomes.
text_fields
text_fields
arrow_upward
VIII pair - the vestibular cochlear nerve consists only of sensory fibers and corresponds to the dorsal root of the spinal nerves.
V, VII, IX and X pairs of cranial nerves
text_fields
text_fields
arrow_upward
V, VII, IX and X pairs - the trigeminal, facial, glossopharyngeal and vagus nerves contain sensory fibers and are homologous to the dorsal roots of the spinal nerves. Like the latter, they consist of neurites of cells of the sensory ganglia of the corresponding nerve. As part of these cranial nerves, there are also motor fibers related to the visceral apparatus. The fibers passing through the trigeminal nerve innervate the muscles derived from the muscles of the first visceral, jaw arch; in the composition of the facial - derivatives of the muscles of the II visceral, hyoid arch; in the glossopharyngeal - derivatives of the I branchial arch, and the vagus nerve - derivatives of the mesoderm II and all subsequent branchial arches.
XI pair - accessory nerve
text_fields
text_fields
arrow_upward
XI pair - the accessory nerve consists only of the motor fibers of the branchial apparatus and acquires the significance of the cranial nerve only in higher vertebrates. The accessory nerve innervates the trapezius muscle, which develops from the muscles of the last branchial arches, and the sternocleidomastoid muscle, which is isolated from the trapezius in mammals.
III, VII, IX, X pairs of cranial nerves
text_fields
text_fields
arrow_upward
III, VII, IX, X cranial nerves also contain myelin-free parasympathetic fibers of the autonomic nervous system. In the III, VII and IX nerves, these fibers innervate the smooth muscles of the eye and the glands of the head: salivary, lacrimal and mucous membranes. The X nerve carries parasympathetic fibers to the glands and smooth muscles of the internal organs of the neck, chest and abdominal cavities. This length of the branching area of the vagus nerve (hence its name) is explained by the fact that the organs innervated by it at the early stages of phylogenesis lay near the head and in the region of the branchial apparatus, and then gradually moved back during evolution, pulling the nerve fibers behind them.
Branching of the cranial nerves. All cranial nerves, with the exception of IV, branch off from the base of the brain ().
III pair - oculomotor nerve
text_fields
text_fields
arrow_upward
III pair - the oculomotor nerve (item oculomotorius) is formed by neurites of the cells of the nucleus of the oculomotor nerve lying in front of the central gray matter of the aqueduct (see Atl.). In addition, this nerve has an accessory (parasympathetic) nucleus. The nerve is mixed, it comes out to the surface of the brain near the anterior edge of the bridge between the legs of the brain and enters the orbit through the supraorbital fissure. Here, the oculomotor nerve innervates almost all the muscles of the eyeball and upper eyelid (see Atl.). After the entry of the nerve into the orbit, parasympathetic fibers leave it and go to the ciliary node. The nerve also contains sympathetic fibers from the internal carotid plexus.
IV pair - trochlear nerve
text_fields
text_fields
arrow_upward
IV pair - the trochlear nerve (item trochlearis) consists of the fibers of the nucleus of the trochlear nerve located in front of the aqueduct. The axons of the neurons of this nucleus pass to the opposite side, form a nerve and come out to the surface of the brain from the anterior cerebral sail (). The nerve bends around the leg of the brain and through the superior orbital fissure enters the orbit, where it innervates the superior oblique muscle of the eye (see Atl.).
V pair - trigeminal nerve
text_fields
text_fields
arrow_upward
V pair - the trigeminal nerve (item trigeminus) appears on the surface of the brain between the bridge and the middle legs of the cerebellum with two roots: large - sensitive and small - motor (see Atl.).
The sensory root consists of neurites of sensory neurons of the trigeminal ganglion, which is located on the anterior surface of the temporal bone pyramid, near its apex. Entering the brain, these fibers terminate in three switching nuclei located: in the lining of the bridge, along the medulla oblongata and the cervical spine, on the sides of the aqueduct. The dendrites of the trigeminal ganglion cells form three main branches of the trigeminal nerve (hence its name): the orbital, maxillary and mandibular nerves, which innervate the skin of the forehead and face, teeth, the mucous membrane of the tongue, mouth and nose cavities (see Atl .; Fig. 3.28 ). Thus, the sensory root of the V pair of nerves corresponds to the dorsal sensory root of the spinal nerve.
Rice. 3.28. Trinity nerve (sensory root):
1 - mesencephalic nucleus; 2 - the main sensory core; 3 - IV ventricle; 4 - spinal nucleus; 5 - mandibular nerve; 6 - the maxillary nerve; 7 - the orbital nerve; 8 - sensory root; 9 - trigeminal ganglion
The motor root contains the processes of the cells of the motor nucleus, which lies in the cover of the bridge, medial to the switching upper sensory nucleus. Having reached the trigeminal node, the motor root passes it, is part of the mandibular nerve, leaves the skull through the foramen ovale and supplies all the chewing and other muscles developing from the jaw arch with its fibers. Thus, the motor fibers of this root are of visceral origin.
VI pair - abducens nerve
text_fields
text_fields
arrow_upward
VI pair - abducens nerve (item abducens), consists of the fibers of the cells of the nucleus of the same name, which lies in the rhomboid fossa. The nerve comes out to the surface of the brain between the pyramid and the bridge, penetrates through the supraorbital fissure into the orbit, where it innervates the external rectus muscle of the eye (see Atl.).
VII pair - facial nerve
text_fields
text_fields
arrow_upward
VII pair - facial nerve (n. facialis), consists of fibers of the motor nucleus lying in the tire of the bridge. Together with the facial nerve, the intermediate nerve is examined, the fibers of which are attached to it. Both nerves exit to the surface of the brain between the pons and the medulla oblongata, lateral to the abducens nerve. Through the internal auditory opening, the facial nerve, together with the intermediate one, penetrates into the canal of the facial nerve, penetrating the pyramid of the temporal bone. In the canal of the facial nerve lies geniculate ganglion - sensitive ganglion of the intermediate nerve. It gets its name from the bend (knee) that forms the nerve in the bend of the canal. Having passed the canal, the facial nerve is separated from the intermediate one, leaves through the styloid opening into the thickness of the parotid salivary gland, where it splits into terminal branches, forming a "big crow's feet" (see Atl.). These branches innervate all facial muscles, the subcutaneous muscle of the neck and other muscles derived from the mesoderm of the hyoid arch. Thus, the nerve belongs to the visceral apparatus.
Intermediate nerve consists of a small number of fibers that extend from geniculate ganglion, lying in the initial part of the facial canal. Entering the brain, these fibers end in the lining of the bridge (on the cells of the nucleus of a single bundle). The dendrites of the cells of the geniculate node are part of the tympanic string - the branches of the intermediate nerve, and then join the lingual nerve (branch of the V pair) and innervate the taste (mushroom and leaf-shaped) papillae of the tongue. These fibers, carrying impulses from the organs of taste, are homologous to the dorsal roots of the spinal cord. The rest of the fibers of the intermediate nerve are parasympathetic, they originate from the superior salivary nucleus. These fibers reach the pterygopalatine node.
VIII pair - vestibular cochlear nerve
text_fields
text_fields
arrow_upward
VIII pair - vestibular cochlear nerve (item vestibulocochlearis), consists of sensitive fibers of the cochlear nerve and the nerve of the vestibule.
Snail nerve conducts impulses from the organ of hearing and is represented by cell neurites spiral knot, lying inside the bone cochlea.
The nerve of the vestibule carries impulses from the vestibular apparatus; they signal the position of the head and body in space. The nerve is represented by cell neurites vestibule node, located at the bottom of the internal auditory canal.
The neurites of the vestibule and cochlear nerve are connected in the internal auditory canal into the common vestibular cochlear nerve, which enters the brain next to the intermediate and facial nerves lateral to the olive of the medulla oblongata.
The fibers of the cochlear nerve end in the dorsal and ventral auditory nuclei of the pons operculum, the nerve fibers of the vestibule - in the vestibular nuclei of the rhomboid fossa (see Atl.).
IX pair - glossopharyngeal nerve
text_fields
text_fields
arrow_upward
IX pair - glossopharyngeal nerve (item glossopharyngeus), appears on the surface of the medulla oblongata, outside of the olive, with several roots (from 4 to 6); from the cranial cavity comes out with a common trunk through the jugular opening. The nerve consists mainly of sensitive fibers that innervate the grooved papillae and the mucous membrane of the posterior third of the tongue, the mucous membrane of the pharynx and middle ear (see Atl.). These fibers are dendrites of the cells of the sensitive nodes of the lingopharyngeal nerve located in the region of the jugular foramen. The neurites of the cells of these nodes end in the switching nucleus (single bundle), under the bottom of the fourth ventricle. Some of the fibers pass to the posterior nucleus of the vagus nerve. The described part of the glossopharyngeal nerve is homologous to the dorsal roots of the spinal nerves.
The nerve is mixed. It also contains motor fibers of gill origin. They start from the motor (double) nucleus of the medulla oblongata and innervate the muscles of the pharynx. These fibers represent the nerve of the first branchial arch.
The parasympathetic fibers that make up the nerve originate from the lower salivary nucleus.
X pair - vagus nerve
text_fields
text_fields
arrow_upward
X pair - vagus nerve (n. vagus), the longest of the cranial, leaves the medulla oblongata behind the glossopharyngeal with several roots and leaves the skull through the jugular foramen together with pairs IX and XI. The ganglia of the vagus nerve are located near the opening, giving rise to it sensitive fibers(see Atl.). Having descended along the neck as part of its neurovascular bundle, the nerve is located in the chest cavity along the esophagus (see Atl.), And the left one gradually shifts to the anterior surface, and the right one to its posterior surface, which is associated with the rotation of the stomach in embryogenesis. Having passed along with the esophagus through the diaphragm into the abdominal cavity, the left nerve branches on the anterior surface of the stomach, and the right one is part of celiac plexus.
Sensory fibers of the vagus nerve innervate the mucous membrane of the pharynx, larynx, root of the tongue, as well as the hard membrane of the brain and are dendrites of the cells of its sensitive ganglia. Cell dendrites terminate in the nucleus of a single bundle. This nucleus, like the double nucleus, is common to the nerves of pairs IX and X.
Motor fibers the vagus nerve branch off from the cells of the double nucleus of the operculum of the medulla oblongata. The fibers belong to the nerve of the II branchial arch; they innervate the derivatives of its mesoderm: the muscles of the larynx, palatine arches, soft palate and pharynx.
The bulk of the fibers of the vagus nerve are parasympathetic fibers originating from the cells of the posterior nucleus of the vagus nerve and innervating the viscera.
XI pair - accessory nerve
text_fields
text_fields
arrow_upward
XI pair - accessory nerve (item accessorius), consists of fibers of cells of the double nucleus (common with the IX and X nerves), which lies in the medulla oblongata outside the central canal, and the fibers of its spinal cord nucleus, which is located in the anterior horns of the spinal cord for 5-6 cervical segments. The roots of the spinal nucleus, having folded into a common trunk, enter through the foramen magnum into the skull, where they join the roots of the cranial nucleus. The latter, 3–6 in number, emerge behind the olive, located directly behind the roots of the X pair.
From the skull, the accessory nerve exits along with the glossopharyngeal and vagus nerves through the jugular foramen. Here the fibers of it inner branch pass into the vagus nerve (see Atl.).
enters the cervical plexus and innervates the trapezius and sternocleidomastoid muscles - derivatives of the branchial apparatus (see Atl.).
The main components of the peripheral nervous system are nerves that connect the central nervous system to other parts of the body, and ganglia- groups of nerve cells (nodes) located at different points in the nervous system
Nerve
Is a bundle of motor (motor) and sensory (sensory) fibers together with connective tissue and blood vessels. Large nerves (43 of them) actually originate from the nervous system: 12 pairs leave the lower part of the brain (cranial nerves) and 31 pairs - from the spinal cord (spinal nerves).
Cranial nerves - nerves, the roots of which are connected to the brain stem. They serve mainly the sensory organs and muscles of the head, although a very important cranial nerve is the vagus ( X steam) - serves the digestive organs, heart and air passages in the lungs. Certain cranial nerves, such as the optic nerve to the eye ( II steam), contain only sensory fibers.
Thus, a person has 12 pairs of cranial nerves that exit at the base of the brain:
I - olfactory (n ervus olfactorii),
II - visual (n. Opticus),
III - oculomotor (n. Oculomotorius),
IV - block (n. Trochlearis),
V - trigeminal (n. Trigemenus),
VI - discharge (n. Abducens),
Vii - facial (n. Facialis),
VIII - auditory, or vestibular cochlear (n. Vestibulocochlearis),
IX - glossopharyngeal (n. Glossopharyneus),
X - wandering (n. Vagus),
XI - additional (n. Accesorius),
XII - sublingual (n. Hypoglossus).
Of them:· three pairs - sensory (sensitive) - I, II, VIII,
· six pairs - motor (motor) - III, IV, VI, VII, XI, XII,
· three pairs - mixed - V, IX, X.
All these nerves innervate the muscles of the face, larynx, pharynx, tongue and partly the neck, and the vagus nerve - the muscles of the internal organs.
Sensory fibers of the cranial nerves are the peripheral parts of the olfactory, visual, gustatory, auditory and skin analyzers; when they are damaged, pain and other sensory disorders appear. Inflammatory processes, trauma, tumors, strokes and some other pathological processes can cause various symptoms of cranial nerve damage - paresis, paralysis, neuropathy and neuralgia, neuritis.
Paresis- weakening, paralysis- complete absence of motor functions with the absence or decrease in muscle strength as a result of various pathological processes in the nervous system, causing a violation of the structure and function of the motor analyzer. Depending on the level of the lesion, central and peripheral paralysis are distinguished.
Neuropathies(neuropathia ) - the general name for lesions of peripheral nerves due to intoxication, hypovitaminosis, autoimmune processes, etc.
Neuralgia(neuralgia ) - acute pain localized within one, less often several peripheral nerves. Neuralgias are caused by various exogenous and endogenous causes: acute and chronic infections (flu, tonsillitis, malaria, tuberculosis), intoxication with various poisons (lead, arsenic, mercury, alcohol). Often, neuralgias appear with chronic intoxications due to gastrointestinal disorders, with diabetes; can occur in the presence of chronic toxic-infectious foci (gynecological diseases, tonsillitis), with gout and hypertension. In some cases, they step on the basis of injury.
The main symptom of neuralgia is subjectively felt and acutely arising paroxysmal pains ("burns", "pricks", "shoots"), which are accompanied by paresthesias (chills, numbness, cold).
An objective examination reveals "pain points" at the site of the exit of the nerve; hyperesthesia, vasomotor-secretory disorders in the form of redness or paleness, sweating or dry skin are often observed. If neuralgia passes into the stage of neuritis or accompanies it, then objective sensory disorders appear, to which reflex-motor disorders can also join. Neuralgias usually take the form of seizures of greater or lesser duration.
Neuritis(neuritis ) - inflammation of the peripheral nerves. It occurs as a result of infections, intoxications, injuries, as well as nutritional disorders, blood circulation, vitamin deficiencies. It is manifested by pain, sensitivity disorders, paralysis, paresis.
Polyneuritis(polyradiculoneuritis) - multiple neuritis, in the process of which the cranial nerves are sometimes involved: IX and III couples (glossopharyngeal and oculomotor) - with diphtheria, Vii pair (facial) - for acute viral polyneuritis, bulbar nerves (motor cranial nerves located in the medulla oblongata ( bulbus ), i.e. sublingual ( XII pair), wandering ( X pair) and glossopharyngeal ( IX couple) - with acute ascending paralysis of Landry. The vagus (X pair) and phrenic nerves are often affected.
Ipair - olfactory nerve
With defeat, there is hyposmia(decreased sense of smell), or anosmia(lack of smell). As a rule, they are one-sided. When the temporal cortex is irritated (for example, by a volumetric process), olfactory hallucinations appear - dysosmia and parosmia.
There is also a pathology called olfactory agnosia(not recognizing familiar smells).
The function of smell is examined using various aromatic substances (mint drops, perfume, ethyl or camphor alcohol), while the nasal passages are closed in turn. You can not use ammonia and other substances with pungent odors, since the trigeminal nerve ( V couple) can react by irritating their branches, that is, the appearance of pain.
IIpair - optic nerve
When the optic nerve is completely interrupted, amaurosis(blindness). Due to various pathological processes, amblyopia or hemiambliopia(decreased visual acuity due to toxic damage to the orbital part of the optic nerve; in the second case, visual damage occurs in opposite fields), hemianopsia(loss of visual fields), which is characterized by blindness of the external (temporal) or internal visual fields (there are several types of hemianopsia, which differ depending on the degree of nerve damage), scotomas- loss of fields of view by sectors.
When the visual cortex (occipital lobe) is irritated, visual hallucinations occur. With damage to the outer surface of the occipital lobe (on the left - in right-handers and vice versa), and visual agnosia- the patient loses the ability to recognize objects by their appearance.
Color blindness(violation of color perception) is detected using multicolor tables.
Studies of visual acuity are carried out using Kryukov tables (letters of decreasing size), the study of visual fields - using the perimeter. Fields of vision can be checked by stretching a towel in front of the patient, which must be divided in half (in the presence of hemianopsia, the patient divides the towel into unequal parts) or using a slit lamp. Of no small importance in neurology is the study of the fundus, the data of which can provide valuable information about the presence of a pathological focus in the brain (volumetric processes).
IIIpair - oculomotor nerve
This nerve provides movement of the eyeball and innervates the muscle that constricts the pupil and carries out the reaction of the pupils to light.
When this nerve is damaged, the following symptoms may appear: ptosis(drooping of the upper eyelid), diplopia up and in, mydriasis(pupil dilation), exophthalmos(standing eyeballs from orbits), as well as exotropia and violation of the convergence reaction(the ability to bring the eyeballs to the bridge of the nose) and accommodation(the ability to clearly see objects that are closer to the distant point of clear vision; accommodation disorders are caused by paralysis of the ciliary muscle).
Symptoms of oculomotor nerve damage can be: anisocoria(difference in pupil size), nystagmus complete immobility pupil, loss of pupillary responses to light - friendly constriction of the pupils.
IVpair - trochlear nerve
It innervates the muscle that turns the eyeball downward and outward.
When damaged, the following symptoms occur: diplopia(double vision) when looking down, i.e. under your feet, and convergent squint... It is extremely rarely affected in isolation, most often due to exacerbation of chronic otitis media.
VIpair - abducens nerve
It innervates the muscle that abducts the eyeball outward.
When defeated, appears convergent squint, diplopia(double vision) when looking towards the affected muscle (outward), inability to turn the eyeball outward.
When defeated, there is isolated paralysis the rectus muscle of the eye, which leads to converging strabismus, diplopia (the inability to turn the given eye outward), especially when looking towards the affected muscle; sometimes - to dizziness and a forced position of the head.
Nuclear damage is accompanied by paralysis(or paresis) of the facial muscles and central paralysis of the limbs ( Fauville symptom), It is also possible gaze paralysis in the direction of the affected muscle and the focus.
To study the function of these nerves, a neurological malleus is used, with the help of which the mobility of the eyeballs is checked (it is suggested to look up, down, outward, inward). Pay attention to the width and uniformity of the palpebral fissures and to the shape and size of the pupils.
The reaction of the pupils to light is checked with a flashlight or with your palms, first closing your eyes tightly, and then quickly removing one of your hands.
Neuropathies III, IV and VI pairs of cranial nerves (oculomotor, block and abducens) are considered together, because their functions are normally interrelated. Nerves are often affected simultaneously or apart with a fracture of the base of the skull, basal arachnoiditis, encephalitis, bone pathology in the orbit, cavernous sinusitis, diabetes mellitus, mushroom poisoning, tumors. With joint paralysis of this group of nerves ( ophthalmoplegia totalis) eye movement is completely excluded.
Vpair - trigeminal nerve
The name of this nerve is due to the fact that it has three branches:
1. ocular,
2. maxillary and
3. mandibular nerves,
which supply nerve endings to the scalp, forehead, nose, upper and lower eyelids, cheeks and lips, as well as teeth, mucous membranes of the nose, gums, tongue and chewing muscles.
Due to the fact that the trigeminal nerve is mixed, when it is damaged, sensitive (hypesthesia, hyperesthesia or pain) and movement disorders (paralysis of the chewing muscles). There are severe paroxysmal pains in the innervation of this nerve - in one or more of its branches. This pathology is called trigeminal neuralgia, which is a common disease. The cause may be pathological processes leading to a narrowing of the holes through which the branches of the nerve enter the cranial cavity. These are local diseases (paranasal sinuses of the nose, ear, eyes, teeth; purulent processes of the skin and subcutaneous tissue of the face; periostitis, herpetic ganglioneuritis), general infections, facial trauma, and in elderly patients - atherosclerosis of the vessels in the face. Other causes include multiple sclerosis.
Pain in the area of this nerve, simulating neuralgia, can be observed with tumors of the middle cranial fossa, neuromas of the trigeminal nerve, arachnoiditis of the base of the brain. The process is localized not only in the peripheral part of the nerve, but, often, in its central segments. The disease arises both as a result of irritation of the nerve itself, and during various processes, in particular, angiospasms in the gasser's node.
Only one of the three branches of the nerve may be affected, but neuralgia of two or all three branches is possible. Pain associated with organ diseases can sometimes radiate to the area of innervation of the trigeminal nerve. abdominal cavity, uterus.
The trigeminal nerve is rich in vegetative fibers, and therefore the main manifestation of the disease serve intense and burning painful paroxysms in the innervation zone of the affected branch(branches) lasting from several seconds to 1-2 minutes, repeating from several to tens of times a day. They are often accompanied by gustatory paresthesias, pain tics, vegetative-vascular disorders: hyperemia and edema of the face, increased secretion of saliva, lacrimation, impaired sweating, nasal congestion, pain in the heart, increased blood pressure, and sometimes photophobia.
Trigger points are found on the face (in the supraorbital, infraorbital and chin openings - the exit point of the trigeminal nerve - its I, II and III branches), the irritation of which causes an attack of pain. Depending on the localization of the process (neuropathy III branches of the nerve) at the same time spasms of the facial muscles are possible - paresis of the masticatory muscles.
A pain attack can be triggered external influences(touch, wind, loud sound), facial expressions while eating, laughing, coughing, talking, vivid emotions. Characterized by a chronic course of the disease with increasingly frequent exacerbations, in connection with which there is a gradual asthenization of patients.
Viipair - facial nerve
In the face area, it forms many branches, the so-called "crow's feet", and innervates all facial muscles, and also gives branches for the anterior third of the tongue and salivary glands.
Facial nerve damage causes paralysis of facial muscles, which, depending on the cause of the occurrence, is called neuropathies(neuritis, paralysis) facial nerve.
Facial nerve neuropathy (neuropathea (neuritis) n. facialis ) - the most common disease among mononeuropathies. In most cases, against the background of infection and cooling, the nerve is compressed in a narrow bone canal, followed by its ischemia and degenerative changes. Compression is facilitated by the congenital narrowness of the canal or its outlet. Sometimes the disease is preceded by local infections (mumps, exacerbation of chronic otitis media) or trauma to the parotid region.
Independently, neuropathy occurs due to an infectious lesion of the inner ear; with syphilitic diseases of the brain (basilar specific meningitis, limited meningitis of the base of the brain). Of the infections, rheumatism, flu are noted (as a complication, this disease can be included in the picture of postinfluenza encephalitis), viral infections(acute polio). From organic diseases, one should bear in mind tumors (primarily of the cerebellopontine angle), multiple sclerosis. In children, it occurs with poliomyelitis and in cases of birth trauma.
The clinical picture is based on movement disorders in the form of weakness and atrophy of all facial muscles of the face, usually on one side.
Due to the greater strength of the muscles of the intact half of the face, its asymmetry arises: on the side of the paresis, a fold on the forehead does not form, the forehead does not wrinkle, the eyebrow does not rise; the nasolabial fold is smoothed; wider palpebral fissure, does not close when the eyes are closed ( lagophthalmos – lagophthalmus ), lacrimation is observed, the eyeball moves up (bell phenomenon). When grinning, the mouth is pulled to the healthy side, the patient cannot whistle, etc., the cheek is swollen, the corner of the mouth is lowered, while eating, solid food gets between the gum and the cheek, and liquid food is poured over the edge of the mouth on the side of the lesion. Asymmetry and stiffness of the paretic side are enhanced with mimic movements: smile, laughter, cry, conversation.
On the affected side, painful sensations, paresthesias, vasomotor-trophic disorders. In most cases, with high damage to the nerve, there is hyperacusis(increased perception of sound, especially low tones), taste disturbance in the anterior 2/3 of the tongue and dry mouth.
It is necessary to distinguish the peripheral nature of the lesion from the central one. At peripheral(extracranial) lesion, unilateral nerve palsy is noted and suffers the whole half of the face... At central(intracranial, basal) paralysis affects only the lower branch - from the cerebral cortex to the nerve nucleus (unilateral damage to the region of the central part of the cortical analyzer or pathways accompanying, for example, hemiplegia). The nucleus or fibers of the facial nerve can be involved in the pathological process in the brain stem (vascular, infectious, oncological), while the innervation of only the lower part of the face is disturbed and occurs paresis of the lower half of one side of the face, while the patient is able to close his eyes and wrinkle the forehead on the affected side.
The disease begins suddenly: paresis develops within a few hours or days. Partial restoration of nerve function occurs within the first week, complete - within 2 months in 2/3 of cases. In 1/3 of patients, after 4-6 weeks, a complicated form of the disease with contracture and an increase in the tone of some facial muscles and involuntary movements on the sick side arising at the time of eating, smiling, laughing and other facial actions is formed.
The contracture is accompanied by unpleasant sensations of constriction and tension, which intensify with excitement, physical stress, in the cold.
In a neurological examination, already during an external examination, attention is paid to the symmetry of the face. For a more detailed check of the functions of the facial nerve, the patient is asked to collect folds on the forehead ("be surprised"), frown ("get angry"), close his eyes ("tightly, as if soap had gotten in"), puff out his cheeks, bared teeth, smile and whistle ( or "blow out the match").
Clarification of the diagnosis of neuropathy and the identification of the prognosis of recovery are facilitated by classical electrodiagnostics with the measurement of the excitability of the branches of the nerve and facial muscles for different types of current and electromyography.
It is necessary to carefully examine the ear, the paranasal cavities; conduct an epidemiological analysis, since the disease often occurs due to infections.
VIIIpair - auditory, or vestibular cochlear nerve
This pair of nerves unites two functionally different sensory nerves, one of which, the cochlear (auditory), provides the perception of sounds, and the other, the vestibular, regulates balance and orientation of the head and body in space. Thus, the nerve has two branches: the truly auditory and vestibular parts of the nerve.
Violation cochlea(auditory ) parts leads to hearing impairments: hypacusia(hearing loss) anacusions(deafness - hearing loss), or hyperacusis(increasing the perception of sounds).
With pathology vestibular part of the nerve arises vestibular ataxia: the balance of the body is upset (tilts and falls in the direction of the defeat) and coordination of movements, appears dizziness, vomit and nystagmus(involuntary rhythmic twitching of the eyeballs, especially when they are abducted, in a horizontal, vertical or rotational plane).
NeuropathyVIIInerveoccurs as a result of intoxication with various substances (for example, a number of antibiotics), as a complication of influenza infection, trauma to the skull, in the vascular process in the vertebrobasilar basin and neurinoma of the nerve trunk.
The function of the auditory nerve is investigated by otolaryngologists, but in neurology, if necessary, whisper speech is checked (alternately on both sides) at a distance of 6 meters. In this case, the words are called, which contain loud consonants ("forty-six", "artillery", etc.). If the patient does not hear from 6 meters, then the distance should be reduced until the patient hears the named words.
The presence of nystagmus is determined by examining the movements of the eyeballs: when they are retracted to the sides (horizontal nystagmus) and up (vertical nystagmus).
With irritation of the temporal lobe cortex, auditory hallucinations occur, even complex ones (patients hear music, various voices). violation of taste in the posterior third of the tongue or on the side of the affected nerve, anesthesia(loss of sensitivity) of the mucous membrane of the pharynx and tongue, dysphagia(violation of swallowing) - since the vagus nerve is also involved in the innervation of the pharynx.
At unilateral dysfunction of the parotid salivary gland, dry mouth may be absent or insignificant, since this function is compensated by the work of the remaining salivary glands.
Glossopharyngeal nerve neuropathy - a rare disease, usually manifested by a syndrome of neuralgia with severe paroxysms of pain lasting from several seconds to 1-3 minutes - in the pharynx, tonsils and the posterior third of the tongue irradiating to the ear. unilateral lesion is noted drooping soft palate, uvula deflection(to the healthy side), dysphonia(hoarseness) dysphagia(swallowing disorder).
At bilateral defeat occurs aphonia(the voice becomes whispering, soundless), when eating, appears choke and cough, liquid food is poured out through the nose. Cardiovascular and respiratory activity is impaired, which can result in the death of the patient.
Research methodology IX and X pairs of cranial nerves include examination of the state of the soft palate: normally it is located symmetrically and, when the letter "a-a-a" is pronounced, it rises equally on both sides; uvula location: normally it is in the midline. The patient is offered to drink a few sips of water or to swallow saliva - swallowing should be free, without choking.
XIpair - accessory nerve
It innervates the sternocleidomastoid muscle (turning the head to the sides - opposite to the nerve) and the trapezius muscle (movements of the scapula and clavicle when they are lifted and pulled back).
Nerve damage leads to paresis or paralysis of these muscles, which is expressed in their atrophy: turning the head in a healthy direction is difficult (torticollis formation is possible), shrugging the shoulders, abducting the shoulder blades to the spine, raising the arms above the horizontal line is limited.
When examining, the patient should normally perform all these movements without difficulty.
Occasionally there are muscle cramps innervated by the XI nerve; they are more often unilateral or are the result of cortical or subcortical irritations. Tonic the spasm gives a picture of "torticollis"; clonic- twitching of the head in the opposite direction, sometimes with simultaneous lifting of the shoulder. Bilateral clonic spasm leads to nodding of the head ( Salaamova spasm).
XIIpair - hypoglossal nerve
The defeat of this nerve leads to paresis or paralysis the corresponding half of the language and is accompanied by atrophy and thinning muscles of the tongue deviation him in the direction of defeat and dysarthria(speech disorder: it becomes tangled and indistinct - "porridge in the mouth"). To test the function of the hypoglossal nerve, the patient is asked to stick out his tongue. Normally, it should be located in the midline. (glossopharyngeal, vagus and sublingual) leads to the so-called bulbar paralysis, which is characterized by the presence of "three D":
- Dysphonia(nasal, nasal tone of voice or hoarseness);
- Dysarthria(articulation disorder - slurred speech, characteristic difficulty in pronouncing some letters - "l", "s", "b", "p");
- Dysphagia(disorder of chewing and swallowing - choking when eating, getting liquid food in the nose).
Atrophy of the muscles of the tongue with fibrillar twitching, paresis of the soft palate is noted. Sensitivity is not upset. Facial ( Vii pair) and trigeminal ( V couple) nerves, as a result of which the patient's face is amimic, the mouth is open, saliva flows out of it.
At bilateral defeat, all of the above pathology takes place in full ("three A"):
- Aphonia(almost silent, whispering speech);
- Anartria(serious disorder of articulation, up to the inability to speak);
- Afagia(serious disorder of swallowing up to the impossibility of performing the act of swallowing).
As an independent disease, bulbar paralysis is rare; it usually joins amyotrophic lateral sclerosis and syringomyelia, when the disease process also affects the bulbar part of the brain. This must be borne in mind when recognizing, like tumors of the medulla oblongata, syphilis, pseudobulbar paralysis due to bilateral damage to the cortical pathways in the brain. Infectious diseases of the brain, poliomyelitis and encephalitis, also accompanied by bulbar paralytic disorders, always develop very acutely.
1.I pair of cranial nerves - olfactory nerve
The pathway of the olfactory nerve consists of three neurons. The first neuron has two types of processes: dendrites and axons. The ends of the dendrites form olfactory receptors located in the mucous membrane of the nasal cavity. The axons of the first neurons pass into the cranial cavity through the ethmoid plate, ending in the olfactory bulb on the bodies of the second neurons. The axons of the second neurons make up the olfactory tract that travels to the primary olfactory centers.
The primary olfactory centers include the olfactory triangle, the anterior perforated substance, and the transparent septum. In these centers, the bodies of the third neurons are located, on which the axons of the second neurons end. Axons of third neurons end in the cerebral cortex of the opposite side, in the cortical olfactory projection areas. These areas are located in the parahippocampal gyrus, in its hook.
Symptoms of the lesion depend on the level of damage to the pathway of the olfactory nerve. The main symptoms are anosmia, hyposmia, hyperosmia, dysosmia, and olfactory hallucinations.
Highest value anosmia and unilateral hyposmia are assigned. This is due to the fact that in most cases, bilateral hyposmia and anosmia are caused by acute or chronic rhinitis.
The loss or decrease in the sense of smell is the result of damage to the olfactory nerve up to the olfactory triangle. In this case, the first or second neuron of the pathway is affected. The defeat of the third neuron does not lead to a violation of the olfactory function, since this neuron is located in the cerebral cortex on both sides. Olfactory hallucinations are the result of irritation of the olfactory projection field, which can be with tumor formations in the hippocampus. A violation of the sense of smell can be a consequence of pathological processes at the base of the skull. This is due to the close location of the base of the skull and the olfactory pathways.
2. II pair of cranial nerves - optic nerve
The first three neurons of the visual pathway are located in the retina. The first neuron is represented by rods and cones. The second neurons are bipolar cells.
Ganglion cells are the third neurons of the pathway. Their axons form the optic nerve, which enters the cranial cavity through the optic opening in the orbit. In front of the Turkish saddle, the nerve forms the optic chiasm. Only part of the optic nerve fibers intersects. After the crossover, the optic fibers are called the optic tract. Due to the intersection of fibers, each optic tract contains visual fibers from the same halves of the retina of the right and left eyes. The fibers of the optic tract end in the external geniculate body, the cushion of the thalamus, in the upper hillocks of the quadruple. Part of the fibers from the upper mounds of the quadruple ends on the neurons of the accessory nucleus of the oculomotor nerve, where the fourth neuron is located. Its axons go to the ciliary node, then to the sphincter of the pupil.
In the external geniculate body, the next neuron is located, the axons of which form the Graziole bundle. This bundle ends in the cells of the cerebral cortex located in the region of the groove on the inner surface of the occipital lobe.
In this area of the cerebral cortex, the optic fibers come to an end, coming from the same halves of the retina of the right and left eyes.
Symptoms of defeat. Decreased vision (amblyopia) or blindness on the side of the optic nerve. The pupil's reaction to light is preserved. When a part of the neurons of the pathway is damaged in the retina or in the optic nerve, a scotoma is formed. It is characterized by the loss of any part of the visual field. Scotoma can be positive or negative. The development of bilateral blindness indicates damage to the optic fibers at the site of their intersection.
Possible damage to the optic fibers located medially and making a complete intersection, there is a loss of the outer half of the visual field on both sides (the so-called bitemporal hemianopsia), or binosal hemianopsia (loss of half of the visual field from the inner side of both eyes with damage to a part of the optic fibers located laterally) ... The appearance of a homonymous hemianopsia (loss of the field of view from the side of the same name) is possible.
This pathology occurs when the optic tract, the external geniculate body, the posterior leg of the internal capsule, the Graziole bundle, and the spur sulcus are affected. Irritation of the area of the cerebral cortex, where the cortical visual representation is located, causes the patient to feel sparks, a flash of lightning, and luminous points (photopsia).
With optic neuritis, its peripheral part, the fibers located in the retina of the eye, and the retrobulbar region are damaged (due to infections, poisoning, alcoholism).
3. III pair of cranial nerves - oculomotor nerve
The pathway of the nerve is two-neuronal. The central neuron is located in the cells of the cortex of the precentral gyrus of the brain. The axons of the first neurons form the cortical-nuclear pathway, heading to the nuclei of the oculomotor nerve, located on both sides.
In the brain, there are five nuclei of the oculomotor nerve, in which the bodies of the second neurons are located. These nuclei are small- and large-celled. The nuclei are located in the midbrain at the level of the upper hillocks of the quadruple in the cerebral peduncles. From the nerve nuclei, the outer muscles of the eye, the muscle that lifts the upper eyelid, the muscle that constricts the pupil, and the ciliary muscle are innervated. All fibers coming from the nuclei of the oculomotor nerve leave the cerebral peduncles, pass through the dura mater, the cavernous sinus, leave the cranial cavity through the superior orbital fissure and enter the orbit.
Symptoms of defeat. Damage to the nerve trunk leads to paralysis of all oculomotor muscles. When a part of the large cell nucleus is damaged, the innervation of the outer muscle of the eye is disrupted. Complete paralysis or weakness of this muscle is clinically observed.
In case of complete paralysis, the patient cannot open his eyes. With weakness of the muscle that lifts the upper eyelid, the patient partially opens the eye. If the large cell nucleus of the oculomotor nerve is affected, the muscle that lifts the upper eyelid is affected last, divergent strabismus or external ophthalmoplegia is observed when only the external muscles are damaged.
Damage to the oculomotor nucleus is often accompanied by the development of alternating Weber's syndrome, which is associated with the simultaneous damage to the fibers of the pyramidal and spinothalamic pathways. The clinical manifestations are joined by hemiplegia on the side opposite to the lesion. Damage to the nerve trunk is characterized by external and internal ophthalmoplegia. Internal ophthalmoplegia is accompanied by the appearance of mydriasis, anisocoria, impaired accommodation and pupil response to light. Mydriasis occurs as a result of paralysis of the sphincter of the pupil.
4. IV pair of cranial nerves - trochlear nerve
The pathway is two-neural. The central neuron is located in the cortex of the lower part of the precentral gyrus. The axons of the central neurons end in the cells of the nucleus of the block nerve on both sides. The nucleus is located in the brain stem in the region of the lower hillocks of the quadruple. There are peripheral neurons of the pathway.
Nerve fibers located from the central to the peripheral neuron make up the cortical-nuclear pathway. Fibers emanating from the nucleus of the block nerve intersect in the region of the cerebral velum. Then the fibers of the block nerve go out behind the lower hillocks of the quadruple and leave the brain substance, pass through the cavernous sinus. The nerve through the superior orbital fissure enters the orbit, where it innervates the superior oblique muscle of the eye. When this muscle contracts, the eyeball rotates downward and outward.
Symptoms of defeat. An isolated lesion of the IV pair of cranial nerves is extremely rare. Clinically, damage to the block nerve is manifested by a restriction of the mobility of the eyeball outward and downward. Since the innervation of the superior oblique muscle of the eye is disturbed, the eyeball is turned inward and upward. With this pathology, double vision (diplopia) will be characteristic, which occurs when looking down and to the sides.
5.V pair of cranial nerves - trigeminal nerve
He is mixed. The sensory pathway of a nerve is made up of neurons. The first neuron is located in the lunate node of the trigeminal nerve, located between the sheets of the dura mater on the anterior surface of the pyramid of the temporal bone. The axons of these neurons form a common root of the trigeminal nerve, which enters the pons of the brain and ends on the cells of the nucleus of the spinal cord, which is a superficial type of sensitivity. In this nucleus, the oral and caudal parts are distinguished: the oral is responsible for the innervation of the region of the face closest to the midline, the caudal part for the areas farthest from this line.
The lunate node contains neurons responsible for deep and tactile sensitivity. Their axons pass through the brainstem and end on neurons in the nucleus of the midbrain pathway, located in the lining of the pons.
Deep and tactile sensitivity of the face is provided by fibers from the opposite side, passing over the midline. In both sensory nuclei, the second neurons of the sensory pathway of the trigeminal nerve are located, the axons of which are part of the medial loop and go to the opposite side, ending in the thalamus, where the third neuron of the trigeminal nerve is located. Axons of third neurons end in the lower sections of the post- and precentral gyri.
The sensory fibers of the trigeminal nerve form three branches: the optic, maxillary and mandibular nerves. The maxillary nerve has two branches: the zygomatic nerve and the pterygopalatine nerves.
The zygomatic nerve provides innervation to the skin of the zygomatic and temporal regions. The number of pterygopalatine nerves is variable and ranges from 1 to 7. Sensory fibers of the maxillary nerve innervate the mucous membrane of the nasal cavity, tonsils, pharyngeal vault, soft and hard palate, main sinus, posterior ethmoid cells.
An extension of this nerve is the infraorbital nerve, which, through the infraorbital foramen, enters the face, where it divides into its terminal branches. The infraorbital nerve is involved in the sensitive innervation of the skin of the lower eyelid, the outer wing of the nose, the mucous membrane and skin of the upper lip to the corner of the mouth, the mucous membrane of the vestibule of the nose. The mandibular nerve is mixed. It innervates the chewing muscles with motor fibers.
Sensory fibers innervate the chin, lower lip, floor of the mouth, anterior two-thirds of the tongue, teeth of the lower jaw, skin of the lower cheek, anterior part of the auricle, eardrum, external auditory canal and dura mater.
Symptoms of defeat. In case of damage or damage to the nucleus of the spinal tract, a segmental type of sensitivity disorder develops. In some cases, a loss of pain and temperature sensitivity is possible while maintaining deep types of sensitivity, such as a feeling of vibration, pressure, etc. This phenomenon is called dissociated sensitivity disorder. In the case of irritation of the motor neurons of the trigeminal nerve, trismus develops, that is, the tension of the masticatory muscles of a tonic nature.
With inflammation of the facial nerve, pain appears in the affected half of the face, which is more often localized in the ear and behind the mastoid process. Less commonly, it is localized in the area of the upper and lower lips, forehead, and lower jaw. In the event of damage to any branch of the trigeminal nerve, the sensitivity of one or more species in the innervation zone of this branch is disturbed. With damage to the optic nerve, the superciliary and corneal reflexes disappear.
A decrease or complete disappearance of the gustatory sensitivity of the anterior 2/3 of the tongue on one side indicates a lesion of the mandibular nerve on the side of the same name. Also, with damage to the mandibular nerve, the mandibular reflex disappears. Unilateral paresis or paralysis of the masticatory muscles occurs when the motor nucleus of the trigeminal nerve or the motor fibers of the mandibular nerve are damaged on the same side.
In the case of bilateral damage to the same nerve formations, the lower jaw drops. Disorder of various types of sensitivity in the areas of innervation of all branches of the V pair of cranial nerves is characteristic of the defeat of the lunate node or the root of the trigeminal nerve. A distinctive feature of the defeat of the lunate node is the appearance of herpetic eruptions on the skin.
The motor nuclei of the trigeminal nerve receive innervation from the central neurons of the cerebral cortex on both sides. This explains the absence of a violation of chewing when the central neurons of the cortex are damaged on one side. Violation of the act of chewing is possible only with bilateral damage to these neurons.
6. VI pair of cranial nerves - abducens nerve
The pathway is two-neural. The central neuron is located in the lower part of the precentral gyrus cortex. Their axons terminate in cells of the abducens nerve nucleus on both sides, which are peripheral neurons. The nucleus is located in the pons of the brain. Axons of peripheral neurons leave the brain between the bridge and the pyramid, bend around the back of the sella turcica, pass through the cavernous sinus, the superior orbital fissure, and enter the orbit. The abducens nerve carries out the innervation of the external rectus muscle of the eye, with the contraction of which the eyeball turns outward.
Symptoms are clinically characterized by the appearance of converging strabismus. A typical complaint of patients is ghosting, located in the horizontal plane. Gübler's alternating syndrome often joins with the development of hemiplegia on the side opposite to the lesion.
Most often, there is a simultaneous defeat of the III, IV and VI pairs of cranial nerves, which is associated with the presence of some anatomical features of their location. The fibers of these nerves are closely located with the fibers of other pathways in the brain stem.
With the defeat of the posterior longitudinal bundle, which is an associative system, internuclear ophthalmoplegia develops. Simultaneous lesions of the oculomotor nerves are associated with their close location to each other in the cavernous sinus, as well as to the optic nerve (the first branch of the trigeminal nerve), the internal carotid artery.
In addition, the simultaneous damage to these nerves is associated with their close location when leaving the cranial cavity. When pathological processes appear on the base of the skull or basal surface of the brain, in most cases, an isolated lesion of the abducens nerve occurs. This is due to its large extent at the base of the skull.
7. VII pair of cranial nerves - facial nerve
He is mixed. The motor pathway of the nerve is two-neuronal. The central neuron is located in the cerebral cortex, in the lower third of the precentral gyrus. The axons of the central neurons are directed to the facial nerve nucleus, located on the opposite side in the pons of the brain, where the peripheral neurons of the motor tract are located. The axons of these neurons make up the root of the facial nerve. The facial nerve, passing through the internal auditory opening, is sent to the temporal bone pyramid, located in the facial canal. Further, the nerve leaves the temporal bone through the styloid foramen, entering the parotid salivary gland. In the thickness of the salivary gland, the nerve divides into five branches that form the parotid nerve plexus.
The motor fibers of the VII pair of cranial nerves innervate the facial muscles of the face, the striatus muscle, the muscles of the auricle, the skull, the subcutaneous muscle of the neck, the digastric muscle (its posterior abdomen). In the facial canal of the pyramid of the temporal bone, three branches extend from the facial nerve: the large stony nerve, the staped nerve, and the tympanic string.
The large petrosal nerve runs in the pterygopalatine canal and ends in the pterygopalatine node. This nerve innervates the lacrimal gland by forming an anastomosis with the lacrimal nerve after being interrupted in the pterygopalatine node. The greater stony nerve contains parasympathetic fibers. The striatal nerve innervates the striatus muscle, causing its tension, which creates conditions for the formation of better audibility.
The drum string innervates the front 2/3 of the tongue, responsible for the transmission of impulses with a variety of gustatory stimuli. In addition, the drum string carries out parasympathetic innervation of the sublingual and submandibular salivary glands.
Symptoms of defeat. When motor fibers are damaged, peripheral paralysis of the facial muscles develops on the affected side, which is manifested by facial asymmetry: half of the face on the side of the nerve lesion becomes immobile, mask-like, the frontal and nasolabial folds are smoothed, the eye on the affected side does not close, the palpebral fissure expands, the angle of the mouth is lowered down ...
Bell's phenomenon is noted - turning the eyeball upward when trying to close the eye on the affected side. Paralytic lacrimation is observed due to the absence of blinking. Isolated paralysis of the facial muscles is characteristic of damage to the motor nucleus of the facial nerve. In the case of attachment of the lesion of the radicular fibers to the clinical symptoms, the Miyar-Gubler syndrome (central paralysis of the limbs on the side opposite to the lesion) is added.
With the defeat of the facial nerve in the cerebellopontine angle, in addition to paralysis of the facial muscles, there is a decrease in hearing or deafness, the absence of a corneal reflex, which indicates a simultaneous defeat of the auditory and trigeminal nerves. This pathology occurs with inflammation of the cerebellopontine angle (arachnoiditis), acoustic neuroma. The accession of hyperacusis and a violation of taste indicate damage to the nerve before the large petrosal nerve leaves it in the facial canal of the temporal bone pyramid.
The defeat of the nerve above the tympanic string, but below the discharge of the staped nerve is characterized by a disorder of taste, lacrimation.
Paralysis of facial muscles in combination with lacrimation occurs when the facial nerve is damaged below the discharge of the tympanic string. Only the cortical-nuclear pathway may be affected. Clinically, there is paralysis of the muscles of the lower half of the face on the opposite side. Often hemiplegia or hemiparesis on the side of the lesion joins the paralysis.
8.VIII pair of cranial nerves - vestibular cochlear nerve
The nerve consists of two roots: the cochlear, which is the lower, and the vestibular, which is the upper root.
The cochlear part of the nerve is sensitive, auditory. It starts from the cells of the spiral node, in the cochlea of the labyrinth. The dendrites of the cells of the spiral node go to the auditory receptors - the hair cells of the organ of Corti.
The axons of the cells of the spiral node are located in the internal auditory canal. The nerve passes in the pyramid of the temporal bone, then enters the brain stem at the level of the upper part of the medulla oblongata, ending in the nuclei of the cochlear part (anterior and posterior). Most of the axons from the nerve cells of the anterior cochlear nucleus cross, passing to the other side of the brain pons. A minority of axons are not involved in crossing.
The axons end on the cells of the trapezius body and the upper olive on both sides. Axons from these structures of the brain make up a lateral loop ending in the quadruple and on the cells of the medial geniculate body. The axons of the posterior cochlear nucleus cross in the midline of the bottom of the IV ventricle.
On the opposite side, the fibers connect to the axons of the lateral loop. The axons of the posterior cochlear nucleus end in the lower hillocks of the quadruple. The part of the axons of the posterior nucleus, not participating in the crossover, is connected to the fibers of the lateral loop on its side.
Symptoms of defeat. If the fibers of the auditory cochlear nuclei are damaged, hearing impairment does not occur. With damage to the nerve at various levels, auditory hallucinations, irritation symptoms, hearing loss, and deafness may appear. Decreased hearing acuity or deafness on one side occurs when the nerve is damaged at the receptor level, when the cochlear part of the nerve and its anterior or posterior nuclei are damaged.
Symptoms of irritation in the form of a whistling, noise, and crackling sensation may also be added. This is due to irritation of the cortex of the middle part of the superior temporal gyrus by various pathological processes in this area, for example, tumors.
The vestibule part. In the internal auditory canal is the vestibular node formed by the first neurons of the pathway of the vestibular analyzer. The dendrites of neurons form the receptors of the labyrinth of the inner ear, located in the membranous sacs and in the ampullae of the semicircular canals.
The axons of the first neurons make up the vestibular part of the VIII pair of cranial nerves, located in the temporal bone and entering through the internal auditory opening into the brain substance in the region of the cerebellopontine angle. The nerve fibers of the vestibular part end on the neurons of the vestibular nuclei, which are the second neurons of the pathway of the vestibular analyzer. The nuclei of the vestibular part are located at the bottom of the V ventricle, in its lateral part, and are represented by the lateral, medial, superior, and inferior.
The neurons of the lateral nucleus of the vestibular part give rise to the vestibular-spinal pathway, which is part of the spinal cord and ends on the neurons of the anterior horns.
The axons of the neurons of this nucleus form a medial longitudinal bundle located in the spinal cord on both sides. The course of the fibers in the bundle has two directions: descending and ascending. Descending nerve fibers are involved in the formation of a part of the anterior cord. Ascending fibers are located to the nucleus of the oculomotor nerve. The fibers of the medial longitudinal bundle are connected with the nuclei of the III, IV, VI pairs of cranial nerves, due to which impulses from the semicircular canals are transmitted to the nuclei of the oculomotor nerves, causing the movement of the eyeballs when the position of the body changes in space. There are also bilateral connections with the cerebellum, reticular formation, and the posterior nucleus of the vagus nerve.
Symptoms of the lesion are characterized by a triad of symptoms: dizziness, nystagmus, impaired coordination of movement. There is a vestibular ataxia, manifested by a shaky gait, a deviation of the patient towards the lesion. Dizziness is characterized by seizures lasting up to several hours, which may be accompanied by nausea and vomiting. The attack is accompanied by horizontal or horizontal rotator nystagmus. When a nerve is damaged on one side, nystagmus develops in the direction opposite to the lesion. With irritation of the vestibular part, nystagmus develops in the direction of the lesion.
Peripheral lesions of the vestibular cochlear nerve can be of two types: labyrinthine and radicular syndromes. In both cases, there is a simultaneous violation of the functioning of the auditory and vestibular analyzer. Radicular syndrome of peripheral lesion of the vestibular cochlear nerve is characterized by the absence of dizziness, may manifest itself as an imbalance.
9. IX pair of cranial nerves - glossopharyngeal nerve
This nerve is mixed. The sensory pathway of the nerve is three-neuronal. The bodies of the first neuron are located in the nodes of the glossopharyngeal nerve. Their dendrites end with receptors in the posterior third of the tongue, soft palate, pharynx, pharynx, auditory tube, tympanic cavity, anterior surface of the epiglottis. The axons of the first neurons enter the brain behind the olive and end on the cells of the nucleus of the solitary pathway, which are the second neurons. Their axons intersect, ending at the cells of the thalamus, where the bodies of third neurons are located. Axons of third neurons pass through the posterior pedicle of the inner capsule and end in the cells of the cortex of the lower part of the postcentral gyrus. The motor pathway is two-neural.
The first neuron is located in the lower part of the precentral gyrus. Its axons end on cells of the double nucleus on both sides, where the second neurons are located. Their axons innervate fibers of the stylopharyngeal muscle. Parasympathetic fibers originate from the cells of the anterior part of the hypothalamus, ending on the cells of the lower salivary nucleus. Their axons form the tympanic nerve, which is part of the tympanic plexus. The fibers end on the cells of the ear node, the axons of which innervate the parotid salivary gland.
Symptoms of the lesion include a violation of taste in the posterior third of the tongue, loss of sensitivity in the upper half of the pharynx, and gustatory hallucinations that develop when the cortical projection areas located in the temporal lobe of the brain are irritated. Irritation of the nerve itself is manifested by burning, varying intensity pains in the area of the root of the tongue and tonsils lasting 1-2 minutes, radiating into the palatine curtain, throat, ear. The pain provokes talking, eating, laughing, yawning, head movement. A characteristic symptom of neuralgia in the interictal period is pain around the angle of the lower jaw on palpation.
10.X pair of cranial nerves - vagus nerve
He is mixed. The sensitive pathway is three-neuronal. The first neurons form the nodes of the vagus nerve. Their dendrites end with receptors on the dura mater of the posterior cranial fossa, mucous membrane of the pharynx, larynx, upper trachea, internal organs, the skin of the auricle, the posterior wall of the external auditory canal. The axons of the first neurons end on the cells of the nucleus of the solitary pathway in the medulla oblongata, which are the second neurons. Their axons end on cells in the thalamus, which are the third neurons. Their axons pass through the inner capsule, terminating in the cells of the cortex of the postcentral gyrus.
The motor pathway begins in the cells of the cortex of the precentral gyrus. Their axons end on the cells of the second neurons located in the double nucleus. The axons of the second neurons innervate the soft palate, larynx, epiglottis, the upper part of the esophagus, and the striated muscles of the pharynx. The autonomic nerve fibers of the vagus nerve are parasympathetic. They start from the nuclei of the anterior part of the hypothalamus, ending in the vegetative dorsal nucleus. Axons from the neurons of the dorsal nucleus are directed to the myocardium, smooth muscles of internal organs and blood vessels.
Symptoms of defeat. Paralysis of the muscles of the pharynx and esophagus, impaired swallowing, leading to the ingress of liquid food into the nose. The patient develops a nasal tone of voice, it becomes hoarse, which is explained by the paralysis of the vocal cords. In the case of bilateral lesions of the vagus nerve, aphonia and suffocation may develop. When the vagus nerve is damaged, the activity of the heart muscle is disrupted, which is manifested by tachycardia or bradycardia when it is irritated. These disturbances in the activity of the heart will be expressed in bilateral lesions. In this case, a pronounced violation of breathing, phonation, swallowing, cardiac activity develops.
11.XI pair of cranial nerves - accessory nerve
It consists of two parts: vagus and spinal. The motor pathway is two-neural.
The first neuron is located in the lower part of the precentral gyrus. Its axons enter the brain stem, bridge, medulla oblongata, passing previously through the inner capsule. The nerve fibers divide into two parts, terminating at different levels of the central nervous system. A smaller part of the fibers ends on the cells of the nucleus of the vagus nerve. Most of the fibers terminate at the level of the anterior horns of the CI – CV spinal cord on both sides.
The second neuron consists of two parts - spinal and vagus. The fibers of the spinal cord leave the spinal cord at the CI – CV level, forming a common trunk, which enters the cranial cavity through the foramen magnum. There, the common trunk connects with the fibers of the motor double nucleus of the XI pair of cranial nerves, forming the trunk of the accessory nerve, which emerges through the jugular opening from the cranial cavity. After the exit, the nerve fibers are divided into two branches - internal and external. The internal branch passes into the lower laryngeal nerve. The outer branch innervates the trapezius and sternocleidomastoid muscles.
Symptoms of defeat. With unilateral damage to the nerve, it is difficult to lift the shoulders, the turn of the head in the direction opposite to the lesion is sharply limited. In this case, the head deviates towards the affected nerve. With bilateral nerve damage, it is impossible to make head turns in both directions, the head is thrown back.
When the nerve is irritated, a muscle spasm of a tonic nature develops, which is manifested by the appearance of spastic torticollis (the head is turned towards the lesion). With bilateral irritation, clonic convulsions of the sternocleidomastoid muscles develop, which is manifested by hyperkinesis with the appearance of nodding movements of the head.
12.XII pair of cranial nerves - hypoglossal nerve
For the most part, the nerve is motor, but it also contains a small part of the sensory fibers of the branch of the lingual nerve. The motor pathway is two-neural. The central neuron is located in the cortex of the lower third of the precentral gyrus. The fibers of the central neurons end on the cells of the hypoglossal nerve nucleus from the opposite side, passing before this through the inner capsule of the brain in the region of the pons knee, the medulla oblongata.
Nuclear cells of the XII pair of cranial nerves are peripheral neurons of the pathway. The nucleus of the hypoglossal nerve is located at the bottom of the rhomboid fossa in the medulla oblongata. Fibers of the second neurons of the motor pathway pass through the substance of the medulla oblongata, and then leave it, leaving in the area between the olive and the pyramid.
Motor fibers of the XII pair provide innervation to the muscles located in the thickness of the tongue itself, as well as the muscles that move the tongue forward and downward, upward and backward.
Symptoms of defeat. If the hypoglossal nerve is damaged at various levels, peripheral or central paralysis (paresis) of the muscles of the tongue may occur. Peripheral paralysis or paresis develops in case of damage to the nucleus of the hypoglossal nerve or nerve fibers emanating from this nucleus. In this case, clinical manifestations develop in half of the muscles of the tongue from the side corresponding to the lesion. Unilateral damage to the hypoglossal nerve leads to a slight decrease in the function of the tongue, which is associated with the interlacing of the muscle fibers of both its halves.
More severe is bilateral nerve damage, characterized by glossoplegia (paralysis of the tongue). In the case of damage to the section of the pathway from the central to the peripheral neuron, central paralysis of the muscles of the tongue develops. In this case, there is a deviation of the tongue in a healthy direction. Central paralysis of the muscles of the tongue is often combined with paralysis (paresis) of the muscles of the upper and lower extremities on the healthy side.
