Produced for fresh and old, open and closed traumatic injuries. In some cases, surgical interventions on the tendons are performed to restore the function of the limb in case of paresis and paralysis, congenital defects and developmental disorders. Tendon surgeries include primary and secondary tendon suture, tendon transposition, plasty, shortening and lengthening. Due to certain structural features of the tendons, surgical interventions on them have certain difficulties and require the use of special surgical instruments and a special suture technique.

Operations on the tendons of the upper extremities produced with fresh and old, open and closed traumatic. In some cases, surgical interventions on the tendons are performed to restore the function of the limb in case of paresis and paralysis, congenital defects and developmental disorders.
There are the following operations on the tendons:
- - tendon suture;
- - dissection of the tendon (tenotomy);
- - plastic replacement of the tendon defect;
- - lengthening or shortening of the tendon;
- - transposition (movement of the tendon to restore a particular function of the limb).
Taking into account the time of the surgical intervention, the following are distinguished:
- - primary tendon suture. Optimally - in the first 6-8 hours, in the absence of signs of infection - on the first day after the injury;
- - early delayed tendon suture. Within a month after injury (in case of primary healing);
- - late delayed tendon suture. Within 30 days or more from the date of injury.
Primary tendon surgeries are not performed if there are signs of infection, with crushed wounds, tendon defects, multiple, etc. Surgical interventions are performed only in a clean operating room by a traumatologist who knows the technique of stitching the tendons. After the operation, the patient must be under medical supervision.
Reconstructive surgical interventions on the tendons are performed routinely, after the wound has completely healed and in the absence of signs of infection. In the process of repairing tendons, it is often necessary to carry out combined or multi-stage surgical interventions, including revision of the tendons, their release from cicatricial adhesions, replacement of scar tissue with autografts, etc.
The complexity of surgical interventions on the tendons is due to some of the features of these anatomical structures:
- The tendon is in a state of tension. If its integrity is violated, the muscle contracts and often pulls the central end of the tendon at a considerable distance from the injury site. This feature is especially pronounced when the flexors are damaged. Often, when the integrity of the flexor is violated at the level of the middle or main phalanx of the finger, its central end is found in the palm of the hand, and sometimes in the area of the wrist joint.
- The tendon consists of dense, longitudinally spaced fibers. It is impossible to sew it with a regular seam, since the threads simply cut through the tendon, dividing it into separate fibers. Designed by a large number of complex sutures, including transverse, oblique and loop-like stitching of tendons, in which their eruption is excluded.
- Under mechanical action on the damaged tendon (picking up with a tool, etc.), its end is easily pulled apart, and the loose end of the tendon is not suitable for suturing. During operations, special instruments are used without sharp protrusions and atraumatic needles.
- When suturing damaged ends of the tendon, insufficient or excessive tension is unacceptable. In the first case, diastasis (distance) occurs between the ends and the tendon does not grow together. In the second case, a clavate thickening is formed, which prevents the normal movement of the tendon, and favorable conditions are created for the formation of cicatricial adhesions with the surrounding tissues.
- In some areas, the tendon runs inside the tendon sheath. With excessive trauma to this anatomical formation, the chances of occurrence increase, into which tendons are soldered.
The restoration of the tendons of the fingers and hand is a complex, laborious process that requires a high level of professional training of a traumatologist and a conscious attitude of the patient. It is absolutely unacceptable to unauthorizedly remove the plaster cast, try to move your fingers or strain your arm, unless authorized by a doctor. Such actions can cause an unsuccessful outcome of the operation, significantly complicate and lengthen the recovery period.

Tendons connect the muscles to the bone, and if a cut occurs in the tendon on the finger, the finger itself becomes difficult to bend and unbend. Very often, a finger can be cut with a knife in the kitchen and then the wound begins to bleed a lot. The goal of treatment is to stop the blood and restore the lost flexion and extension function of the finger.
If you cut the tendon on your finger, then your actions are as follows:
- rinse the cut. You can rinse it under cold water with laundry soap or hydrogen peroxide. But you don't need to put your finger under the cold water faucet trying to stop the bleeding. It is best to lift it up for a while after processing and hold it in this position;
- treat the skin around the wound with iodine... Treat the very surface of the wound with hydrogen peroxide. Vishnevsky's ointment, as well as ichthyol ointment, is not suitable here:
- stop the blood. Finely ground coffee powder will instantly stop the blood after injury. Sprinkle it on the cut and bandage it for two days, the wound will heal quickly;
- put a tight bandage on your finger... Ordinary bandaging leads to the fact that the bandage simply slips off, sometimes the bandage dries to the wound and it becomes painful to change the bandage. It is best to wrap your finger at the cut with a ribbon of paper, which will cover the entire phalanx, and then you can already glue the plaster or wrap the bandage. The paper wrapper will protect the wound, move the edges and help it heal faster. Also, the bandage will be more convenient to remove, because the paper will not stick to the wound;
- treat the wound with ointment... After the blood has stopped, you can treat the cut with ointment. It can be a spray or ointment Dexpanthenol or ointment with chamomile and comfrey, as well as ointment with calendula;
You should see your doctor if you have any of the following symptoms:
It is not possible to bend and straighten the finger in any way;
There is severe pain;
The finger is numb;
Finger jamming;
The cut occurred on the back of the finger.
Hospital treatment can be as follows:
 - d the doctor will examine the finger, check its sensitivity, blood flow and finger strength... He can give a referral to a surgeon or orthopedist, without fail sent for an x-ray;
- d the doctor will examine the finger, check its sensitivity, blood flow and finger strength... He can give a referral to a surgeon or orthopedist, without fail sent for an x-ray;
- surgery may be required depending on the type of cut, as severely cut tendons require surgical intervention... The surgeon will sew all the tendons together. It is possible that a special pin will be inserted into the bone, on which the damaged tendon is fixed;
-after the operation, a splint is applied to protect the hands, which is worn for up to two months... After surgery, you will need to restrict your hand movements to speed up the healing process. A physiotherapist will work with the patient to help restore the strength and speed of the arm.
Rehabilitation in case of damage to the tendons of the fingers of the hand is divided into preoperative and postoperative. At the same time, it is necessary to know that preoperative rehabilitation is no less important than postoperative, since it lays the foundation for the success of treatment in general.
Physiotherapy exercises of both damaged and healthy rays, the segment as a whole;
Paraffin applications;
Remedial gymnastics of synergists and injured muscles;
Restoration of passive mobility of the joints, set in motion by the damaged tendon;
Preparing the skin for surgery.
Maintaining passive joint mobility is one of the most important conditions, without which there is no point in restoring the tendon. Most effective method to prevent arthrogenic contracture - splinting an injured finger with a neighboring healthy finger using adhesive plaster rings.
It is more difficult to restore the passive mobility of the finger with an existing contracture. Here passive classes come to the fore. remedial gymnastics... It is carried out for 20-30 minutes several times a day with an intensity that excludes the appearance of pain.
The content of postoperative measures.
In the postoperative period, several time periods are clearly distinguished, during which the rehabilitation effects differ sharply from each other.
1. The period of immobilization. The sutured tendon allows you to recommend active movements from 3-4 days after the postoperative edema subsides. But the frequency, intensity and strength of movements, as well as the movements themselves, are controlled by the operating surgeon. Pain syndrome cannot serve as a criterion when movements are limited or stopped. This is important, since the entire range of possible movements often depends on this period. The duration of the period is on average 3 weeks.
During the specified period, applies technique of single movement of the tendon in the canal with full amplitude... The technique was proposed for the rehabilitation treatment of patients with sutured flexor tendons of the fingers.
1. After the edema subsides, a palmar plaster splint is applied to the operated beam (s) in the position of straightening the finger and flexing in the wrist joint at an angle of 30-35 degrees. After a day, the splint changes to the back one, which fixes the flexion of the finger in all joints during extension in the wrist joint by 30 degrees. A prerequisite is complete active flexion of the finger, performed by the patient independently. After 10-12 days, the splint can be changed more often. The end of the splint change period is the 21st day from the date of the operation.
2. Early postoperative period. At the end of the 3rd week, the tendon (its segments) is fused both with each other and with the surrounding tissues. The scars are still fragile and tendon suture ruptures are possible. The initial movements should be light. Any sudden movements are contraindicated. Preference for sutured flexor tendons is given to flexion movements, with sutured extensors - extension movements. The frequency of movements during the entire period from the 21st to the 35th day after the operation increases and by the end reaches 500-600 movements per day.
3. Period of intensive development. Treatment of a patient in this period, the duration of which is determined only by the effectiveness of the development of active movements, can last from 1 to 5-6 months. During this entire period, the patient must be under medical supervision. This recommendation is most often violated, and subsequently, with regret, one has to state incomplete restoration of movements. A surgeon or a rehabilitation therapist determines a gradual increase in the load, the connection of power devices and the need for electrical and physiotherapy, as well as other additional procedures. Success is possible only if the surgeon, the patient and the rehabilitation physician are united into one whole to achieve the final result. The patient's intellect, his perseverance and persistence in achieving the goal are of paramount importance.
Indications for tendoplasty and its types.
Clinical practice has convincingly shown that the secondary suture of the flexor tendons along the hand does not give good results, since the development of cicatricial processes blocks the movement of the sutured tendon. For this reason, as well as because of diastasis between the ends of the tendon in cases where more than 4 weeks have passed after the injury, tendoplasty is indicated.
The main principle of plastics of the flexor tendons of the fingers of the hand is the removal of the ends of the damaged tendon and its replacement with a tendon graft with the removal of the tendon suture zone outside the bone-fibrous canals. The success of this intervention is ensured only when the following four conditions are met:
1) the full range of passive movements in the joints of the fingers;
2) preservation of the annular ligaments supporting the tendon;
3) the minimum number of scars along the bone-fibrous canals;
4) full-fledged skin.
Depending on the fulfillment of these conditions, three main groups of patients can be distinguished: with favorable, unfavorable and extremely unfavorable conditions for performing tendoplasty.
Conditions favorable for the operation are found in patients with chronic injuries after cut wounds, which were sutured without intervention on the tendons and healed without suppuration. In this case, the joints retain their passive function in full, and the annular ligaments supporting the tendons are not damaged.
Conditions unfavorable for tendoplasty arise if a tendon suture has already been applied in patients (tendoplasty has been performed) or the wound has healed with suppuration. However, with widespread cicatricial changes in the tissues along the bone-fibrous canals, the function of the joints and the supporting tendons of the ligaments is preserved.
Under extremely unfavorable conditions, persistent (often flexion) contractures of the joints of the fingers, damage to the annular ligaments, and cicatricial changes in the skin are added to the widespread scar tissue changes along the bone-fibrous canals. Sometimes these pathological tissue changes are combined with improperly fused (or non-fused) fractures of the phalanges of the finger with a curvature of its axis.
Obviously, the surgeon has a good chance of a successful one-stage tendoplasty under favorable conditions. These chances are significantly reduced in unfavorable conditions and are completely absent in extremely unfavorable situations. This is why the surgeon has no alternative in the latter group: he can only perform tendon reconstruction in two stages. Moreover, during the first stage of the operation, extremely unfavorable (or unfavorable) conditions are translated into favorable ones.
One-stage tendoplasty. In a one-stage tendoplasty, the surgeon sequentially performs:
- excision of the ends of the damaged tendons along the bone-fibrous canal;
- taking a tendon graft;
- introduction of the graft into the osteo-fibrous canal and its fixation to distal phalanx finger and to the central end of the tendon on the forearm.
Tendoplasty should be performed with minimal tissue trauma, including adjacent intact tendons.
Refusal from tendoplasty is possible with chronic injuries of the SGS in the 1st zone and the preserved function of the ATP, when the simplest and most sufficient effective method The solution to the problem is tenodesis (arthrodesis) in the distal interphalangeal joint. Another way is two-stage plastic SGS while maintaining the ATP.
Operation technique. Excision of the ends of the damaged tendons is most often performed using three approaches: along the finger, in the middle part of the hand (most often along the distal palmar groove) and in the lower third of the forearm (Fig. 27.2.22). If necessary, these accesses can be combined.
Rice. 27.2.22. Access schemes (a, b, c), which can be used for plastics of the flexor tendons of the fingers of the hand.
The most important rule This stage of the operation is the dissection of the wall of the osteo-fibrous canal at a minimum extent and only between the annular ligaments. If the latter are damaged, then it is necessary to perform their plastic. Significant difficulties can arise during the removal of the central ends of the CGS into the proximal wound on the forearm. The reason for this is not only the formation of scars in the area of the canal of the wrist, but also the presence of powerful worm-like muscles. If the surgeon does not open the wrist canal (and this is done only for injuries within the 4th zone of the hand), then pulling the central end of the CGS from the access to the forearm leads to rupture of the vermiform muscles and to significant hemorrhage in the tissue (and, consequently, to their subsequent scarring).
Practice has shown that if one or two GHS is damaged, this can be omitted. The central end of the CGS is isolated at the level of the metacarpus in the proximal direction and cut off, and the tendon graft is carried out in a nearby canal formed with the help of a bougie. Then the central end of the graft is fixed to the central end of the CGS, which is crossed on the forearm. With this approach, the graft having a very small cross-section does not lead to compression of the anatomical structures in the wrist canal, while the trauma of this stage of the operation is significantly reduced. This technique is all the more appropriate if damaged superficial tendons are removed from the wrist canal.
Taking a tendon graft. The characteristics of the various sources of tendon grafts and the technique for taking them are set out in Ch. 14. In practice, the surgeon chooses between the tendon of the long palmar muscle (in case of damage to the tendons on one, short, toe) and the tendons of the long extensors of the toes.
It is important to emphasize that the method of transposition of ATP from an adjacent intact finger should not be used, as this is the worst choice of plastic material. The reasons for this are obvious: the tendon is taken from the “critical” zone (!) Of the intact finger, thereby triggering the pathogenetic mechanism of blockade of the SGS remaining on the donor finger by newly formed scars; the balance of the flexor and extensor tendons is disturbed.
The graft is fixed in the region of the distal phalanx in any way that provides sufficient strength. In the forearm, it is preferable to fix it using Pulvertaft or other methods at a distance of at least 3 cm from the entrance to the wrist canal (with straightened fingers). This can be achieved under the following conditions:
- the tourniquet from the upper third of the forearm must be removed;
- the hand should be in the middle physiological position;
- after the final fixation of the graft, the fingers should be positioned so that the more ulnarly located finger is in the position of greater flexion (Fig. 27.2.23).

Rice. 27.2.23. The layout of the fingers of the hand after tendoplasty with the correct length of the graft (explained in the text).
Due to the fact that full flexion of the finger requires significant efforts, and the muscles are always weakened after a long period of inactivity, it is advisable to hem the central end of the ATP of the injured finger (in the "side to side" type) to the central end of the corresponding CG. In this case, the level of the anastomosis should be located 1.5-2 cm proximal to the place where the SGS is stitched with the graft.
Before closing the wound, the zones of tendon anastomoses are wrapped with muscles, if possible, which reduces their subsequent cicatricial fixation to adjacent tendons and to the skin.
Two-stage tendoplasty. Indications. It is well known that one-stage tendoplasty is futile in the following situations:
- with pronounced arthrogenic contractures in the joints of the fingers;
- with extensive cicatricial changes in the skin, when the soft tissues on the palmar surface of the fingers are not enough to restore damaged tendons;
- with concomitant skeletal injuries (fractures and false joints of the phalanges, etc.) with deformation of the lumen of the bone-fibrous canals;
- with extensive defects of soft tissues (extensive scars) in the lower third of the forearm, as well as along the wrist and metacarpus;
- with repeated unsuccessful operations on the flexor tendons.
One-stage tendoplasty is possible, but the chances of good results are drastically reduced under the following conditions:
- if at least one operation on the tendons has already been performed (primary suture, tendoplasty);
- if wound healing was complicated by deep suppuration;
- if the surgeon plans to perform plastic surgery of the SGS while preserving the ATP;
- in case of damage to the annular ligaments of the finger.
Ultimately, the surgeon makes the decision individually, but in all of the above cases, experienced specialists prefer to carry out a two-stage surgery... Under imperfect initial conditions, it provides a higher level of professional guarantees of a good result.
1st stage. Rods. For implantation into the fibrous bone canals of the fingers, rods are used, which are subject to the following requirements:
1) the dimensions of the cross-section of the rod must correspond to the dimensions of the cross-section of the damaged tendon;
2) the rod should be flexible enough so as not to oppose (in the postoperative period) the movements of the fingers;
3) the rod must be made of a biologically inert material so as not to cause an excessive inflammatory reaction of the surrounding tissues.
In our practice, we use polyvinyl chloride rods with an oval cross-section of five standard sizes (Fig. 27.2.24):
6.0 x 3.5 mm; 5.5x3.5mm; 5.0 x 3.0 mm; 4.5x2.3 mm; 4.0x2.5mm
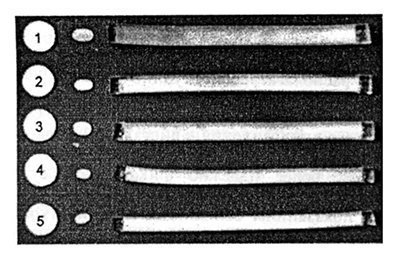
Rice. 27.2.24. Sizes of cross-section of PVC rods (explanation in the text).
The duration of the implantation period is determined by two main factors: 1) the timing of the formation of a connective tissue capsule around the rod and 2) the duration of the recovery period for the full volume of passive movements in the finger joints (in the presence of contractures).
Histological studies have shown that a relatively mature connective tissue capsule around the nail is formed by the end of the 2nd month after surgery. Its morphology is influenced by three main factors: 1) surgical tissue trauma; 2) tissue reaction to the implant; and 3) irritating effect of movements. After a 2-month period, there is a gradual thickening of the capsule with the formation of villous protrusions. Over time, the size of the villi gradually increases. This made it possible to conclude that the minimum period of rod implantation should be 2 months. Subsequently, the quality of the capsule deteriorates.
The second most important criterion for the duration of the rod implantation period is the period of restoration of the full range of passive movements in the finger joints. This task is accomplished using a special technique for developing movements (see section 27.2.6), which often takes a very long time. It is possible to plan the 2nd stage of the operation only after the passive movements in the joints of the finger become not only full in volume, but also sufficiently free.
Rod implantation technique. Operation scheme:
- access;
- excision of the ends of the damaged tendons and the formation of the osteo-fibrous canal;
- (elimination of contractures in the joints of the finger);
- insertion of the rod into the osteo-fibrous canal and fixation of its distal end;
- (plastic of the annular ligaments);
- stopping bleeding, washing the wound with an antibiotic solution and closing it;
- (cross skin plastic);
- fixing the central end of the rod;
- drainage and closure of the forearm wound.
The ends of the damaged tendons are removed along general rules with maximum preservation of the walls of the tendon sheath and annular ligaments. According to indications, contractures of the joints of the fingers are eliminated (redressing, capsulotomy, etc.).
After that, a rod is implanted into the osteo-fibrous canal. Its peripheral end is fixed with a strong immersion suture to dense tissues in the region of the distal interphalangeal joint. In this case, the thread knot should be located in the depth of the wound.
It is advisable to fix the end of the rod so that the distal part of the CGS is preserved in the place of its attachment to the distal phalanx. During the second stage of the operation, this allows for a more reliable fixation of the tendon graft.
According to the indications, the plastic of the annular ligaments is performed. The subsequent closure of the wound should be preceded by the removal of the tourniquet and careful control of bleeding in the wound using a bipolar coagulator. After this procedure, the bone-fibrous canals are washed with a solution of antibiotics (their intravenous administration is started at the beginning of the operation).
A significant difference in the technique of closing wounds of the fingers and hand is the imposition of a two-row suture. A deep row is applied with thread No. 6 / 0-7 / 0 so that there is not even a minimum free space left near the rod. The successful solution of this most important task largely guarantees the subsequent uncomplicated wound healing.
If the soft tissues are not enough (for the imposition of a deep row of sutures), then the tissues of the displaced skin flap (from the adjacent finger) are used or the transposition of the vermiform muscles is carried out.
The second layer - skin sutures - is applied according to the usual methods.
Fixation of the central end of the nail to the end of the corresponding tendon on the forearm is not strictly necessary, but is performed by most surgeons. The application of the rod-tendon anastomosis solves two main tasks. First, the restoration of the kinematic chain makes active finger movements possible (to a limited extent within the framework of the postoperative patient management scheme). This improves the functional state of the muscle and thereby speeds up the rehabilitation period after replacing the rod with a tendon graft.
Secondly, when performing the second stage of the operation, it becomes easier to find the ends of the tendons corresponding to the finger.
The zone of fixation of the rod to the tendons should be located no closer than 5-6 cm from the entrance to the wrist canal. For fixation, 1-2 sutures are applied.
It is important to note that when closing a wound on the forearm, the surface of the rods must be carefully covered with soft tissues, and the wound must be adequately drained.
Practice has shown that the risk of developing infectious complications increases significantly if more than two rods are implanted in the wrist canal area. So essential principle the 1st stage of the operation is the absence of direct contact in the wound of two adjacent implants.
It is important to use the following rule of implant placement. With tendoplasty on one or two fingers, the rods can be installed along the entire length of the tendon: from the distal interphalangeal joint to the lower third of the forearm. With a greater number of injured fingers, each of the additional rods is placed only up to the level of the metacarpus in compliance with the above rules for closing the wound (Fig. 27.2.25).
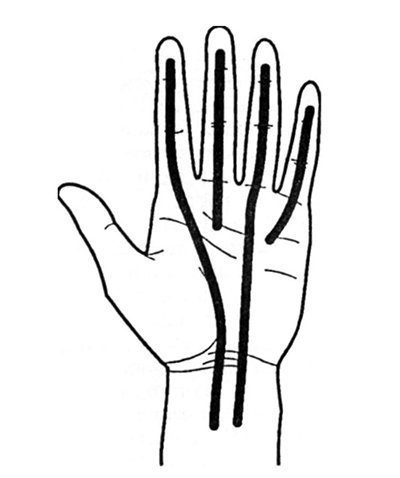
Rice. 27.2.25. Arrangement of rods during their implantation on several fingers of the hand (explanation in the text).
At the end of the operation, the fingers are set in the following positions: 1) with flexion contractures in the joints of the fingers or in the absence of contractures, the fingers are fixed in an extended position with palmar flexion (30 °) in the wrist joint; 2) with extension contractures in the finger joints, the corresponding joints are bent.
In all cases, sufficient blood circulation in the skin must be maintained in all areas of the fingers and hand.
The latter is not always successful with persistent extensor contractures of the metacarpophalangeal joints and requires a special approach (see section 27.10).
2nd stage. Operation technique. Replacing the rod with a tendon graft, as a rule, does not present technical difficulties and is carried out from two small approaches: in the region of the distal interphalangeal joint and in the lower third of the forearm (Fig. 27.2.26).
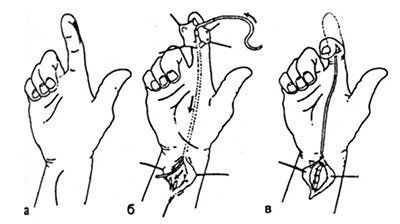
Rice. 27.2.26. Diagram of the stages of replacing an implanted rod with a tendon graft.
a - access lines; b - removal of the rod and insert the graft; c - graft fixation.
The distal end of the rod is found in the tissues of the finger, sutured with a long ligature and brought out into the wound on the forearm. Simultaneously (or sequentially), a tendon graft is introduced into the canal. Particular attention is paid to firm fixation of the distal end of the graft, the separation of which in the postoperative period is a frequent complication. Preference should be given to an unremovable tendon suture, which is more reliable.
When fixing the tendon graft at the level of the forearm, it is necessary to excise those scar tissue that is directly adjacent to the area of the tendon suture.
Postoperative management of patients is carried out according to general principles.
Complications. The most dangerous complication of the first stage of the operation is wound suppuration. The increased risk of developing infectious complications upon implantation of large foreign bodies (rods) in the tissue of the hand requires adherence to a number of rules.
The most important of them are:
- strict adherence to the rules of asepsis and antiseptics during the intervention;
- the use of relatively safe options for the location of the rods in the tissues of the hand;
- suturing of wounds over the exposed surfaces of the rods without the formation of "dead" spaces;
- washing wounds with antibiotics;
- especially careful stopping of bleeding;
- complete rest of the fingers and hands during the first 10-12 days after surgery and a limited load on the rods thereafter;
- full antibiotic therapy in the postoperative period.
Practice shows that with the development of suppuration, removal of the rod is inevitable, and later repeated attempts to restore the tendons are often unsuccessful.
Another common complication is synovitis, or aseptic inflammation of the tissues surrounding the rod, with a pronounced exudative reaction. Its frequency can be 8-16%. Synovitis can turn into suppuration.
Most often, synovitis appears with excessive movements of the operated finger. Therefore, it is advisable to adhere to the following rules for preventing irritation of the tissues surrounding the implanted rod:
- the number of finger movements (active and passive) should be minimal and carried out within the framework of an individual rehabilitation scheme;
- during the entire period between two operations, the brush must be kept warm, sudden cooling and hypothermia are contraindicated.
Tearing off the rods at the distal attachment point can be diagnosed by the absence of active finger movements (if the suture is also applied to the forearm), or by radiographs when rods made with X-ray contrast additives are used.
It should be noted that the position of the PVC rods can be accurately recorded even on conventional radiographs due to their sufficient density. If the rod is torn off, a re-operation is indicated.
Tears of tendon grafts after the second stage of the operation are more common than after one-stage tendoplasty, and can reach 7.6% and 1.1%, respectively. In 75% of cases, the rupture occurs in the region of the distal interphalangeal joint within 2 months after the start of active finger movements.
Treatment tactics depend on the extent of preserved finger function and may involve reoperation.
Special options for two-stage tendoplasty. Implantation of polymer rods can be part of other complex reconstructive procedures. In particular, when the toes are transplanted onto the hand, the insertion of the rod into the canal of the flexor tendons creates more favorable opportunities for the subsequent restoration of function. It also additionally stabilizes bone fragments during osteosynthesis and greatly simplifies the management of the postoperative period.
When transplanting complex flaps to the lower third of the forearm, polymer rods can be passed through the graft tissue for the subsequent 2nd stage of tendon plasty. This is advisable, first of all, in cases when distal and proximal to the tissue flap of the receiving bed, the scar is changed.
IN AND. Arkhangelsky, V.F. Kirillov
