Available at six different levels. Rupture of the extensor tendon aponeurosis within the nail phalanx has various forms.
a) Damage to the distal terminal phalanx. In case of rupture or transection of the extensor tendon bundles (at this level, tendon bundles of the small muscles of the hand predominate), the tone of the deep flexor prevails, the nail phalanx assumes a flexion position.
Due to the fact that long extensor tendon attached more proximally, its function does not fall out completely, so the middle phalanx assumes a position of slight hyperextension. Regarding the mechanism of rupture of the extensor tendon, Kroemer does not share the opinion of most textbooks, according to which damage to the tense extensor tendon occurs with strong flexion of the terminal phalanx.
Characteristic position of the finger in case of damage to the extensor tendon at various levelsIn his opinion, the reason gap is, for the most part, a sudden overextension of the terminal phalanx. Clinical picture damage should be different from fracture-dislocation of the joint. The latter is confirmed by X-ray examination and an attempt to passively extend the nail phalanx, which, as is known, is not carried out during dislocation.
Mek Duncan distinguishes between different types of damage to the extensor aponeurosis at the level of the terminal joint, and he divides them into injuries accompanied by bone avulsion or without it. The prognosis of the first is more favorable, since a bone fragment can grow even after conservative treatment.
 The most common types of rupture of the extensor tendon aponeurosis within the terminal joint according to Witt
The most common types of rupture of the extensor tendon aponeurosis within the terminal joint according to Witt
b) Damage to the extensor aponeurosis in the proximal terminal phalanx. In this case, the function of the long extensor falls out and the terminal phalanx assumes a flexion position, without hyperextension of the middle phalanx.
Treatment for both types of damage basically identical. Most of the authors to this day remain supporters of conservative therapy (Böhler, Homann, Kremer, Rozov, Winterstein, Rauber). The main principle of any method of conservative treatment is the immobilization of the terminal phalanx in a state of hyperextension for 4-6 weeks. L. Böhler and his students use a plaster or celluloid case to fix the finger in a state of hyperextension, in which a hole is cut out according to the place of the nail, the middle joint is left free. Many surgeons also fix the middle joint of the finger.
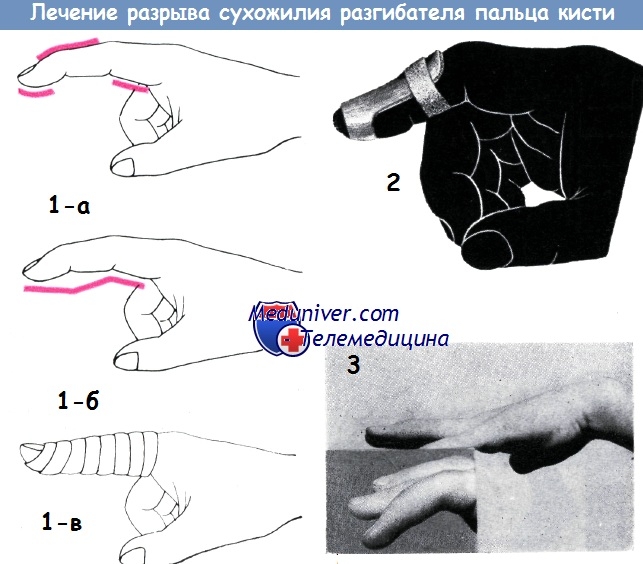 1 a-c - Kremer's method for the treatment of rupture of the extensor tendon within the terminal phalanx
1 a-c - Kremer's method for the treatment of rupture of the extensor tendon within the terminal phalanx 2 - Winterstein tire
3 - 8-year-old girl, after an injury of the ring finger of the left hand during the game, could not straighten the terminal phalanx of the finger.
The doctor was consulted two weeks after the injury, at the same time a splint bandage was applied, the phalanx was given a hyperextension position. Finger function returned to normal after 6 weeks
Pratt recommended " internal splinting e" when fixing the transcutaneous terminal phalanx with a Kirschner wire in the hyperexthesia position and the middle phalanx in the flexion position. Previously, the channel through which the pin was passed was infected in 20% of cases (bone and articular panaritium), but at present, infection is practically not observed. Lengenhager proposes the use of an adhesive bandage that holds the terminal phalanx in the hyperextension position and the middle phalanx in the flexion position. However, the adhesive bandage does not provide sufficient fixation for such a long period.
 Tire Rozova, used without a bandage for the treatment of rupture of the extensor tendon
Tire Rozova, used without a bandage for the treatment of rupture of the extensor tendon
Kroemer prefers conservative method of treatment: Imposes a lined aluminum splint and adhesive bandage for six weeks. Winterstein proposed the use of a metal tire, which Rauber still considers to be the method of choice. A dorsal metal splint, shaped like a segment of a circle, extends from the middle phalanx to the edge of the nail. It must be modeled individually for each patient according to the plaster cast, as otherwise it leads to pressure sores.
The splint is reinforced with a circular motion of a waterproof adhesive patch so that the tip of the finger remains free. Duration of fixation is 6-8 weeks. Rozov's method resembles the one just described.
 "Internal splinting" using Kirschner wires to hold the finger in the hyperextension position. The diagram shows two crossed spokes (1) and one located along the axis of the bone (2)
"Internal splinting" using Kirschner wires to hold the finger in the hyperextension position. The diagram shows two crossed spokes (1) and one located along the axis of the bone (2)
The only difference is that fixation instead of a sticky patch, it is achieved by the tire itself due to its case-like shape. Rauber with conservative treatment for 2-3 weeks, and Winterstein 6 weeks achieved good results.
On the based on personal experience we cannot agree with this, since in patients who come to us a few weeks after the injury, we could not achieve any results with immobilization, with the exception of one eight-year-old child in whom treatment was started 2 weeks after the injury.
 Sewing of the aponeurosis of the extensor tendon, torn off together with the bone fragment from the place of attachment, according to Bunnell (a).
Sewing of the aponeurosis of the extensor tendon, torn off together with the bone fragment from the place of attachment, according to Bunnell (a). X-ray picture of a similar operation we performed (b)
According to I. Böhler, in the case of conservative treatment, flexion in the middle joint is a necessary condition, since sufficient fixation of the end joint cannot otherwise be achieved by either a plaster cast or splinting.
However, from middle joint fixation in the flexion position can be abandoned in the case of operative fixation using the crossed-wire method used for arthrodesis of the finger joints. I. Böhler's reports are known about this method. Personally, I have applied it in 17 cases without complications. The needles are inserted on both sides from the edges of the nail towards the midline of the finger when the joint is hyperextended.
In the presence of old(more than three weeks) rupture of the extensor tendon successfully only surgical treatment. When opening the wound between the ends of the tendon, a discrepancy of 2-3 mm is found, filled with scar tissue. The scar is to be removed. The central end of the tendon is sutured to the distal end by the Bunnell method using a thin stainless wire (or nylon thread).
Thread ends are pulled out at the distal edge and tied over it. When applying a wire suture, the use of a central “pulling” suture is also required. After three weeks, the stitches are completely removed. When the tendon is torn from the place of attachment, accompanied by a detachment bone tissue apply transosseous suture. I. Böhler immobilization of the joint, even after suturing, is carried out by cross-wire fixation with a duration of up to 5 weeks.
Since the application submersible crossed spokes does not threaten the risk of infection, this method is the most acceptable for immobilization of the terminal phalanx. In our five patients with similar injuries, the cure also occurred without complications. Iselen uses a free tendon graft for an old rupture of the extensor tendon. This method leads to better results than re-suturing the tendon.
Finger injuries are common in sports that involve the hands. These types primarily include volleyball, basketball, handball, baseball. With proper treatment, most of these injuries usually heal without significant problems. Such injuries include damage, which is called the "hammer finger". Most commonly, this injury occurs when a ball strikes an extended finger unexpectedly, causing the tip of the finger to flex violently and excessively. As a result, the tendon of the extensor muscle of the fingers is injured in the region of the last interphalangeal joint, which leads to the inability to straighten the fingertip. A finger with a curved tip becomes like a hammer. With timely and proper treatment, complete healing of the tendon occurs and mobility in the joint returns. If the injury has not been given due attention, a permanent deformity of the finger develops, which is called the "hammer finger".
Anatomy
Interphalangeal joints are block-shaped - movement is possible only in one plane. Flexion and extension are carried out by contraction of the flexor and extensor muscles of the fingers, respectively. These muscles are located on the forearm, and their tendons branch out in the area of the palm and back and stretch to the fingers. See Hand Anatomy for more details.
Mechanism of injury
Most often, a hammertoe injury occurs when a ball strikes an outstretched finger unexpectedly, resulting in sharp and excessive flexion of the tip (Fig. 1). As a result, the extensor tendon of the fingers is injured at the distal interphalangeal joint.
Pathological anatomy of injury
There are three degrees of injury "hammer finger" (Fig. 2):
- the tendon is stretched beyond its elasticity, which leads to micro-tears in the tendon tissue, but it is not completely torn
- complete rupture of the tendon of the extensor muscle of the fingers
- avulsion fracture - the tendon is torn off with a bone fragment of the distal phalanx of the finger.
Symptoms and Diagnosis
the treatment is too painful. When the finger is very weak and with any awkward movement, touching the tip of the finger causes pain (for example, when putting your hand in your pocket). The second case is an avulsion fracture. In this case, the fragments must be fixed. For this, a thin metal pin is used, which is inserted in such a way that it fixes not only fragments, but also the distal interphalangeal joint (Fig. 4).Rehabilitation after an injury
Non-surgical rehabilitation
joint, ensuring its complete immobility lasts from 6 to 8 weeks. If the injury was neglected and not treated for more than 3 months, then the fixation of the joint is extended up to 8-12 months. In the next 6 months, the splint is applied only at night. Due to the constant wearing of the splint, skin problems are possible. If any, it is necessary to change the tire to a new one or use a tire made of a different material. After removing the splint, the doctor will show necessary exercises, which will help restore mobility and smoothness of movement.Rehabilitation after surgery
The main tasks of rehabilitation after surgery are to restore joint mobility, prevent
The invention relates to medicine, namely to hand surgery. A transverse incision is made along the rear of the DMFS, mobilization of the edges of the skin incision and revision of the tendon with transverse excision of the skin with a "petal" 20 mm long, 2-3 mm wide along the rear of the DMFS. The tourniquet is removed from the finger under the control of hemostasis. The skin is sutured with interrupted or U-shaped sutures from non-absorbable suture material. After the wound has healed, the skin sutures are removed, and a control ultrasound examination is performed. When confirming the formation of a tendon regenerate of sufficient strength, the Kirschner wire is removed. 2-3 days after the removal of the spokes, rehabilitation measures are carried out by performing passive and active movements. distal phalanx operated finger with a gradual increase in range of motion over 2 weeks. The method allows you to connect the ends of the tendon without a tendon suture, which allows you to carry out active and passive movements in early dates. 1 pr., 10 ill.
The invention relates to the field of medicine, namely to hand surgery, and concerns methods for repairing ruptures of the extensor tendons of the three-phalangeal fingers of the hand.
Closed ruptures of the extensor tendons in zone I are more common than the other three types combined. In subcutaneous extensor tendon rupture, the degree of distal phalanx extension deficiency can range from a few degrees of limitation to a 75° deficit. The aim of the treatment of tendon injury in zone I is to restore the continuity of the tendon.
There are ways to conservatively treat closed ruptures of the extensor tendons of the fingers at this level up to 4 weeks after injury. These include external fixation of the finger with various splints (Vogt, Rozov, Volkov, Usoltseva, Stark) for 6 weeks and an additional 2 weeks of night wear or 8 weeks of permanent immobilization of the finger. However, the effectiveness of methods of conservative treatment of distal extensor tendon ruptures, according to various authors, does not exceed 50-77%.
Thus, the disadvantages of conservative treatment of fresh closed tears are: a long period of finger immobilization (up to 8 weeks) and inefficiency in 23-50% of cases. Known ways surgical treatment closed ruptures of the extensor tendons of the fingers at the level of the distal interphalangeal joint (DMJ) are temporary arthrodesis of the DMJ finger with a Kirschner wire in the extensor position for 6 weeks and intra-stem sutures with different points of thread fixation, removed tendon sutures with external fixation and temporary arthrodesis of the DMJ with a Kirschner wire.
Despite the relative simplicity of extensor tendon repair techniques, 1/3 of surgical interventions end in unsatisfactory results.
When performing temporary arthrodesis of DMFS without performing a tendon suture after removal of the Kirschner wire 6 weeks after surgery, 25% of patients still have insufficient maturity of the regenerate with ultrasound of the tendon, which requires further immobilization of DMFS.
The disadvantages of the known methods of surgical treatment of this type of injury with the performance of a tendon suture are:
The appearance of marginal necrosis of the skin of the rear area of DMFS after a Z-shaped incision and extensive exposure of the extensor tendon due to poor vascularization of the surface layers of soft tissues in the rear of DMFS;
Slow positive dynamics of the wound process in the postoperative period after extensive mobilization of the skin in the area of the distal interphalangeal joint;
The possibility of rupture of the sutures of the repaired tendons during the initial development of the finger after the cessation of temporary arthrodesis or the formation of an extensor contracture of DMFS, due to the strong tension of the extensor tendon by the intra-trunk tendon suture;
Migration of the suture material from the distal part of the tendon suture, due to the growing nail plate, impaired growth of the nail plate, ligature fistulas;
The need to remove a removable tendon suture 6 weeks after surgery;
The appearance of relapses after the cessation of DMFS fixation.
There was a need to develop new way surgical treatment of a closed rupture of the extensor tendon without performing a tendon suture, but with faster tendon regeneration than with temporary DMFS arthrodesis.
Closest to the present invention is a method of surgical treatment of a closed rupture of the extensor tendon in the I zone, including transarticular temporary arthrodesis DMFS needle Kirchner for 6 weeks. The disadvantages of this method are: the need for further immobilization after removal of the pins in 25% of cases, the lack of the possibility of active development after removal of arthrodesis, the duration of temporary disability.
New technical task- increasing the efficiency of the method due to low traumatization of the area of surgical intervention, reducing the frequency of relapses and unsatisfactory results of the operation, the possibility of active development of DMFS after removal of arthrodesis, reducing the duration of temporary disability.
To solve the problem in the method of repairing closed ruptures of the extensor tendons of the fingers of the hand at the level of the distal interphalangeal joint (DIPJ), including conduction anesthesia of the injured finger with the application of a tourniquet, the formation of a temporary arthrodesis of the DMJ with a Kirschner wire, an additional transverse incision is made along the rear of the DMJ, mobilization of the edges of the skin incision and revision of the tendon with transverse excision of the skin with a “petal” 20 mm long, 2-3 mm wide along the rear of the DMFS, after which the tourniquet is removed from the finger under hemostasis control, the skin is sutured with interrupted or U-shaped sutures from non-absorbable suture material, then, after healing wounds, skin sutures are removed, a control ultrasound examination (ultrasound) is performed, upon confirmation of the formation of a tendon regenerate of sufficient strength, the Kirschner wire is removed, 2-3 days after the removal of the wire, rehabilitation measures are carried out by performing passive and active movements of the distal phalanx of the operated patient calves with a gradual increase in the range of motion within 2 weeks.
Figure 1-10 shows illustrative material for a better understanding of the proposed method.
Fig.1. Complications in the postoperative period after intratubular extensor tendon sutures in zone I.
1 - ligature fistula;
2 - ligature fistula with migration of the suture material of the tendon suture to the nail plate.
Fig.2. Operation scheme.
Fig.3. Conduction anesthesia of the finger according to Oberst-Lukashevich.
Fig.4. Temporary arthrodesis of the DMFS of the second finger of the left hand with a Kirschner wire.
Fig.5. Transverse excision of the skin with a “petal” along the rear of the DMFS of the fourth finger of the right hand.
Fig.6. Mobilization of the skin along the edges of the wound with revision of the tendon of the fourth finger of the right hand.
Fig.7. View of the third finger of the right hand after performing skin sutures.
Fig.8. X-ray after temporary arthrodesis of DMFS of the third finger of the right hand.
Fig.9. Patient K. 3 months after surgery (active extension of the distal phalanx of the fourth finger of the left hand).
Fig.10. Patient K. 3 months after surgery (active flexion of the distal phalanx of the fourth finger of the left hand).
The method is carried out as follows.
Under conduction anesthesia of the injured finger according to Oberst-Lukashevich, a temporary arthrodesis of DMFS is formed with a Kirschner wire and a transverse excision of the skin with a “petal” of 20 × 2-3 mm along the rear of the DMFS is performed, if possible without damaging the veins of the rear of the finger, with mobilization of the edges of the skin incision with scissors with revision of the injury tendon (stretch or tear). The tourniquet is removed from the finger with hemostasis control. The skin is sutured with interrupted or U-shaped sutures with 4/0 non-absorbable suture material. Close the wound with a sterile dressing.
Skin sutures are removed after the wound has healed (8-12 days after the operation). The Kirschner wire is removed 4-6 weeks after the control ultrasound (confirmation of the formation of a tendon regenerate of sufficient strength). Passive and active movements of the distal phalanx of the operated finger can be performed 2-3 days after removal of the pin, with a gradual increase in the range of motion.
Justification of the method
Excision of the skin with a "petal" 20 mm long and 2-3 mm wide is necessary to remove excess skin that appears after skin mobilization from the extensor tendon along the rear of the DMFS. A transverse incision along the rear of DMFS excludes the formation of dermatogenic contracture of DMFS. Mobilization of the skin along the rear of the DMFS with arthrodesis in DMFS allows achieving good contraction of the extensor tendon in zone I and does not require tendon suture. A skin incision with mobilization of the edges from the extensor tendon also causes temporary ischemia of the dorsal region of the DMFS, which stimulates the formation of a tendon regenerate. The method allows to start earlier active rehabilitation. The appointment of rehabilitation measures 2-3 days after the removal of the pin after a control ultrasound confirming the formation of a tendon regenerate of sufficient strength, 2-3 days after the removal of the pin is necessary for more effective rehabilitation and restoration of joint mobility, contributes to the prevention of contractures. The duration of the course of exercises for 2 weeks is sufficient to prevent complications.
B-noy K., 42 years old, was admitted with a diagnosis of finger tendon rupture. Was held surgery according to the proposed method. Under conduction anesthesia of the injured finger according to Oberst-Lukashevich, a temporary arthrodesis of DMFS was formed with a Kirschner wire and transverse excision of the skin with a “petal” of 20 × 2-3 mm along the rear of the DMFS was performed without damaging the veins of the rear of the finger, with mobilization of the edges of the skin incision with scissors with revision of the tendon injury ( stretching or tearing). After that, the tourniquet was removed from the finger with hemostasis control. The skin was sutured with interrupted sutures with a 4/0 non-absorbable suture material. The wound is closed with a sterile napkin.
Skin sutures were removed after wound healing 8 days after surgery. The Kirschner wire was removed 4-6 weeks after the control ultrasound (confirmation of the formation of a tendon regenerate of sufficient strength). 2-3 days after the removal of the pin, it is possible to assign passive and active movements of the distal phalanx of the operated finger with a gradual increase in the range of motion. Discharged on the 10th day without complications.
The inventive method was tested in the clinic ANO "Research Institute of Microsurgery TNTs SB RAMS", 42 patients were operated on in 2010-2011. The course of the postoperative period in patients is smooth. There were no cases of relapse. Perhaps outpatient treatment after surgery.
As a result, the following advantages have been identified in comparison with known operational methods:
Simplicity of the technique and low-impact operation;
Mild postoperative period with rapid relief inflammatory process, pain syndrome;
Absence of a tendon suture;
No need for further immobilization or temporary fixation of DMFS after removal of the Kirschner wire;
The possibility of early recovery of active movements of the distal phalanges of injured fingers in all patients.
The results obtained are achieved, in our opinion, due to a good contraction of the extensor tendon after mobilization of the skin edges in the area of the surgical wound and stimulation of the formation of the tendon regenerate by ischemia in the area of the surgical access.
Sources of information
1. Golubev I.O. Injuries to the extensor tendons of the fingers / Course of plastic surgery: A guide for physicians. In 2 volumes / Ed. K.P. Pshenisnova. - T.II. - Yaroslavl; Rybinsk: Publishing House of OJSC "Rybinsk Printing House", 2010. - P.1345-1362.
2. Gubochkin N.G., Shapovalov V.M. Selected issues of hand surgery. Tutorial. - St. Petersburg: Interline LLC, 2000. - 112 p.
3. Zelenin V.N., Zolotev A.S., Sorokovikov V.A. A method for the treatment of injuries of the extensor tendon of the finger. Patent No. 2334479 C2, 01/10/2008.
4. Zolotov A.S. Features and results of treatment of various variants of distal injuries of the fingers leading to "hammer-shaped deformity" / A.S. Zolotov, V.N. Zelenin // Bulletin of Traumatology and Orthopedics. N.N.Priorova. - 2006. No. 2. - P.81-84.
5. Zolotov A.S. Conservative treatment injuries of the extensor tendons of the fingers / A.S. Zolotov, V.N. Zelenin, V.A. Sorokovikov // Bulletin of Traumatology and Orthopedics. N.N.Priorova. - 2007. No. 9. - P.73-75.
6. Kuzmenko V.V., Korshunov V.F., Eskin N.A., Magdiev D.A., Chulovskaya I.G. A method for restoring the extensor tendons of the fingers in case of their subcutaneous ruptures and open injuries. Patent No. 2188599 C1, 09/10/2002.
7. Magdiev D.A., Chulovskaya I.G., Korshunov V.F., Eskin N.A. Treatment subcutaneous lacerations extensor tendons at the level of the distal interphalangeal joint // Vesti. RSMU. - 2005. - No. 7 (46). - P.25-28.
8. Mikusev G.I. A method for treating damage to the extensor tendon of the finger in the area of attachment to the nail phalanx. Patent No. 2245682 C2, 10/10/2002.
9. Arora R, Lutz M, Gabl M, Pechlaner S. Primary treatment of acute extensor tendon injuries of the hand // Oper. Orthop. Traumatol. 2008. - Mar; 20(1). P.13-24.
10. Doyle J.R. Extensor tendon - acute injuries // In Green D.P., ed. Operative hand surgery, 3rd ed. new york. - Churchill Livingstone, 1993. - P.1925-1954.
11. Geyman J.P., Fink K., Sullivan S.D. Conservative Versus Surgical Treatment of Mallet Finger: A Pooled Quantitative Literature Evaluation // J. Am. Board Fam. Pract. - 1998. - N11: 5. - P.382-390.
12. Jablecki J, Syrko M. Zone 1 extensor tendon lesions: current treatment methods and a review of literature // Ortop. Traumatol. Rehabil. - 2007. - Jan-Feb; N9(1). - P.52-62.
13. Newport M.L., Blair W.F., Steyers S.M. Jr. Long-term results of extensor tendon repair // J. Hand Surg., - 1990. - V.15A. - P.961-966.
14. Newport M.L. Early repair of extensor tendon injuries // In Berger R.A., Weiss A.P. ed. Hand surgery. - Philadelphia. - Lippincott. - 2004. - P.737-752.
15 Stark H.G. A modified splint for mallet finger // J. Hand. Surg. - 1986. - V.11B. - P.236-238.
A method for restoring closed ruptures of the extensor tendons of the fingers of the hand at the level of the distal interphalangeal joint (DMJJ), including conduction anesthesia of the injured finger with the application of a tourniquet, the formation of a temporary arthrodesis of the DMJ with a Kirschner wire, characterized in that an additional transverse incision is made along the rear of the DMJ, mobilization of the edges of the skin incision and revision of the tendon with transverse excision of the skin with a “petal” 20 mm long, 2-3 mm wide along the rear of the DMFS, after which the tourniquet is removed from the finger under hemostasis control, the skin is sutured with interrupted or U-shaped sutures from non-absorbable suture material, then after the wound has healed skin sutures are removed, a control ultrasound examination is performed, upon confirmation of the formation of a tendon regenerate of sufficient strength, the Kirschner wire is removed, 2-3 days after the removal of the wire, rehabilitation measures are carried out by performing passive and active movements of the distal phalanx of the operated finger with gradual increased range of motion for 2 weeks.
