The most acute manifestations of osteochondrosis of the spine are called. Most often, this disease is encountered by people in the age range of 30-60 years. In addition, it has been noticed that men are more likely to be affected by it. We will try to figure out such a disease as a hernia on the spine, whether an operation is needed here and, if so, what kind surgical treatment is it better to choose?
What types of hernia repair operations will you be offered?
There may be several types. The traditional method - discectomy - involves the removal of the disc with the further formation of an immobile connection of a pair of adjacent vertebrae.
Not so long ago, when a herniated disc was removed, a laminectomy was often done. However, this method has some serious drawbacks: for example, a rather large trauma after the surgical approach.
The consequences of this injury became the source of problems during further recovery, when the hernia had already been removed. In particular, it took a long period of time for the lesions to heal, as a result, the muscle of the damaged area noticeably weakened, which caused relapses.
That is why they began to develop methods that provide for reducing the size of the surgical access and, consequently, the injury itself, as much as possible.
Are there more modern types of operations?
 The main significant change was the use of the surgical microscope. Thanks to him, the technique of intra-laminar microsurgical disposal of hernias arose, today it is considered, perhaps, the most optimal method in surgery.
The main significant change was the use of the surgical microscope. Thanks to him, the technique of intra-laminar microsurgical disposal of hernias arose, today it is considered, perhaps, the most optimal method in surgery.
Further, the operation to remove the intervertebral hernia began to be carried out using microsurgical, endoscopic and other methods. At the moment, surgical techniques for the treatment of hernia are developing along this path - the way to reduce the size of the injury during the operation.
Microsurgical operations are performed with special endoscopic instruments. Minimally invasive surgery has several significant advantages when compared to traditional treatments. Tissue trauma during surgery is reduced, and in general, the volume of surgical intervention, as well as the frequency of complications.
When using the endoscopic method, it is possible to significantly reduce the terms of the patient's incapacity for work and their stay in the clinic.
Is laser hernia treatment effective?
 Minimally invasive surgical interventions during the treatment of an intervertebral hernia include microdiscectomy, the use of B-Twin systems, as well as vaporization of the nucleus of the affected area with a laser.
Minimally invasive surgical interventions during the treatment of an intervertebral hernia include microdiscectomy, the use of B-Twin systems, as well as vaporization of the nucleus of the affected area with a laser.
Removal of the intervertebral, despite advertising, cannot be attributed to any extraordinary methods. In this case, the use of lasers even acts as a publicity stunt that speaks of the advancement of medical technologies.
In truth, the beams that are generated by the laser are very difficult to control, which means that there is a danger of damaging nearby internal organs... In addition, the cost of laser surgery will be higher than when using other, less "fashionable" methods.
How is endoscopic microdiscectomy done?
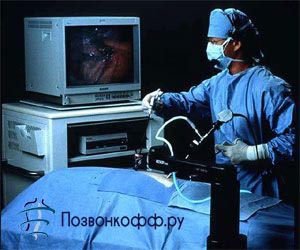 This operation is performed using local anesthesia. In the process, the endoscope (its diameter is 4 mm) is brought to the intervertebral disc of the hernia through a small incision (no more than 0.5 cm), all actions are projected on the screen of a special monitor.
This operation is performed using local anesthesia. In the process, the endoscope (its diameter is 4 mm) is brought to the intervertebral disc of the hernia through a small incision (no more than 0.5 cm), all actions are projected on the screen of a special monitor.
A specialist, under this visual control, removes with a special tool both the hernia itself and the remnants of the nucleus pulposus of the disc; it is worth noting that even a small part of the vertebra is not removed.
This operation is considered less traumatic when compared, for example, with traditional microdiscectomy. This allows you to reduce the risks of complications and reduce the postoperative rehabilitation period. In many cases, the operation is completed by restorative treatment of the operated site with lasers.
An extract from the clinic is made, if not on the day of the operation, then after 1-3 days with the opportunity to engage in non-physical activities practically on the next day after being discharged, and after 2-6 weeks - to physical labor.
How is facet nerve destruction performed?
 Surgery to remove a herniated disc is possible in the form of destruction of the facet nerves. In other words, this is a minimally invasive surgical intervention, which consists in inactivating pain receptors of the intervertebral joints (the second name is facet joints).
Surgery to remove a herniated disc is possible in the form of destruction of the facet nerves. In other words, this is a minimally invasive surgical intervention, which consists in inactivating pain receptors of the intervertebral joints (the second name is facet joints).
This procedure will be more effective if there is a so-called "facet syndrome" - this pain syndrome that occurs during arthrosis of the intervertebral joints.
To confirm this diagnosis, you first need to carry out a special blockade of these nerves. Only in the case of positive dynamics of nerve blocking can radiofrequency destruction of the facet nerves be performed using a radiofrequency probe, which is brought to the nerve by puncture. This procedure is carried out under local anesthesia, it lasts half an hour (the very exposure to radio frequencies is 2 minutes), most often patients tolerate it quite easily, after an hour the patient can go home.
Want to know more about laser vaporization?
 has completely different reviews on the Internet. What is it like? Laser vaporization is an irradiation of an intervertebral disc with a special laser beam in a destructive mode. Such irradiation actually destroys part of the disc: evaporation occurs, which reduces the pressure inside the disc by up to 30% and therefore reduces disc herniation.
has completely different reviews on the Internet. What is it like? Laser vaporization is an irradiation of an intervertebral disc with a special laser beam in a destructive mode. Such irradiation actually destroys part of the disc: evaporation occurs, which reduces the pressure inside the disc by up to 30% and therefore reduces disc herniation.
This technique is often used for patients in the age range of 20-50 years, at an early stage of the lesion of the intervertebral disc. Recall that at an early stage, the protrusion of the annulus fibrosus does not exceed 6 mm. For older patients and in the presence of pronounced degenerative disc changes, this method is not always suitable.
At the same time, such an operation may not be easy curative action but even prophylactic. This is because the disc, which has been vaporized due to the developing fibrosis and sclerosis on it, then does not shift, which means that the risk of hernia progression is noticeably reduced.
This procedure for getting rid of a hernia will take about one to two hours in a hospital, the surgery itself will last from 20 minutes to half an hour.
How is laser disc reconstruction performed?
 This type of intervertebral disc surgery is a non-destructive irradiation of the intervertebral disc with a special laser beam. With such irradiation, the disc heats up, and this stimulates the growth of cartilage cells and restores the patient's intervertebral disc. New cartilage cells in the period from 3 months to six months fill the cracks in the disc, which is why there is an absolute disappearance of acute and even chronic pain in the patient's spine.
This type of intervertebral disc surgery is a non-destructive irradiation of the intervertebral disc with a special laser beam. With such irradiation, the disc heats up, and this stimulates the growth of cartilage cells and restores the patient's intervertebral disc. New cartilage cells in the period from 3 months to six months fill the cracks in the disc, which is why there is an absolute disappearance of acute and even chronic pain in the patient's spine.
This irradiation procedure takes place in the form of a needle puncture of the affected area of the body. The entire treatment process will take from two to three days in a hospital. This procedure can be performed both independently and when the patient has a hernia removed in order to prevent its recurrence.
Do I need surgery for a hernia of the cervical spine?
 If the hernia on the neck is in an advanced stage, then you should resort to surgery. The purpose of such an operation is to decompress not only spinal cord, but also the spinal cord root.
If the hernia on the neck is in an advanced stage, then you should resort to surgery. The purpose of such an operation is to decompress not only spinal cord, but also the spinal cord root.
In the process of removing the cervical disc, it is necessary to stabilize the diseased segment. For this, various special implants are used, and, in addition, prosthetics of the intervertebral disc.

The information on the site is provided for informational purposes only, does not claim to be reference and medical accuracy, and is not a guide to action.
Do not under any circumstances self-medicate. Please consult your doctor!
Tell your friends.
Herniated disc precursors - advanced stage osteochondrosis or injury spinal column... Depending on in which part of the spine the hernial protrusion is localized, the following symptoms occur: headaches, numbness of the upper or lower extremities, deterioration of mobility in the area of the affected disc. In some cases, paresis of the limbs occurs.
It is possible to treat a herniated intervertebral disc conservatively (the use of medications, physiotherapy, massage and exercise therapy) or surgery. Indications for surgery to remove a hernia: prolonged pain syndrome that does not respond to conservative therapy, a large size of the hernial protrusion, which compresses the nerve endings and
Hernias can be localized in the thoracic, cervical or lumbar spine. Regardless of the location of the protrusion, doctors initially resort to gentle methods of therapy, and only when conservative methods have been tried, the neurologist will recommend an operation to remove the hernia. It is advisable to perform the operation if the use of traditional methods of treatment for 1.5–2 months did not give positive results and the pain continues to torment the patient.

In addition to the ineffectiveness of conservative therapy, the indication for surgery is the large size of the hernial protrusion. With a hernia of the thoracic or lumbar spine, surgery is necessary if the size of the protrusion exceeds 9 mm. The indication for immediate surgery is the cauda equina syndrome, which is characterized by severe pain, change in tactile sensations, violation of reflex functions.
The size of the hernial protrusion in the thoracic and lumbar spine up to 5 mm is considered small, up to 8 mm - medium, over this size - these are large hernias, in which it is advisable to perform the operation.
With a hernial protrusion in the cervical spine, the indication for surgery is a protrusion, the size of which exceeds 6 mm. Herniated disc cervical the spine is considered small with sizes up to 2 mm, medium - up to 4 mm, large - up to 6 mm, but even with this size, conservative therapy can be dispensed with. With a hernia over 6 mm, an operation is performed. Surgical intervention is also necessary for spinal stenosis, even if the size of the protrusion is small or medium.
Preoperative diagnostics
As already mentioned, an operation on the spine should be performed with intense pain, which cannot be relieved by conventional therapeutic methods, with large hernial protrusions, with impaired sensitivity and motor activity of the limbs.
Before deciding on an operation, the doctor carefully examines the part of the spinal column in which the disc ruptured with the exit of the nucleus pulposus.
Magnetic resonance imaging is required to determine the location and size of the hernia. This method for examining the intervertebral disc is accurate and informative, but also complex. This method allows you to determine the size and localization of the hernial protrusion and identify concomitant pathological processes.
Also read:
Another study that is used for disc protrusion is computed tomography. However, this technique is not as effective as MRI (errors occur), and is less safe for the patient's body.
If, after treatment with traditional methods, the patient's pain does not stop, dysfunction of the pelvic organs occurs, and the studies have shown a large hernia - surgery is required. There are several methods for removing a pathological neoplasm.
Surgical methods
Before performing an operation on a patient, one should carefully and deliberately approach the choice of a method for removing a hernial protrusion. Excision of a pathological neoplasm is performed in several ways, and they all have their pros and cons. The choice of technique depends on the diagnosis, medical history and patient preference. The financial condition of the patient plays an important role. But more often than not, pain makes the patient agree with the doctor, since the patient's only desire is to get rid of the problem as soon as possible.
There are several ways to perform an operation for disc protrusion and hernial protrusion. This:
- discectomy;
- microdiscectomy;
- laminectomy;
- endoscopy;
- nucleoplasty.
Each of these methods relieves the patient from pathology. The pains subside, and it seems to a person that already tomorrow he can start active activity. But after surgery, rehabilitation is necessary. In addition, it must be remembered that removing a hernia does not promise a 100% result, sometimes pains return, and a relapse occurs.
Discectomy
This method is already outdated, it is necessary to do such an operation in extreme cases. The intervention takes place under general anesthesia - the surgeon makes a 10 cm incision and excises the affected disc. This is an inexpensive option for hernia removal that requires antibiotic therapy and long-term rehabilitation. After the intervention, the operated person stays in the hospital for two weeks. Full rehabilitation takes place in three months.
The advantage of this method is the minimum percentage of relapses (3%).
Microdiscectomy
This is a microsurgical intervention. Through a small incision (up to 4 cm), the surgeon, using a powerful microscope, releases the hernial protrusion and releases the compressed nerve root. After excision of the neoplasm, laser treatment is performed to regenerate damaged disc tissues.
After the microsurgical excision has been performed, the patient is allowed to sit down, and rehabilitation in this case will take no more than a month. The patient is allowed to start vigorous activity with physical exertion after wearing a special supporting corset for three months. The disadvantages of this method are relapses up to 15% in the first postoperative year.
Endoscopy
This microsurgical procedure is performed using endoscopic instruments under epidural anesthesia. The surgeon controls his own actions through the monitor, since the instruments are equipped with a microscopic camera. The incision is minimal (no more than 2 cm). This is a minimally invasive surgery in which the muscles and ligaments remain intact. Already 1-2 days after hernia repair, the patient is allowed to go home, while rehabilitation lasts less than a month. This method has few disadvantages and is therefore often used in surgery.
Cons: the recurrence rate is 10%, not all types of hernias can be removed using endoscopy, and this is an expensive operation.
Nucleoplasty
This minimally invasive procedure is performed under local anesthesia. Look like this - in several places damaged disk small holes are made using a special needle. Laser or radio-frequency radiation is transmitted through the hole of the needle, the gelatinous substance inside the disc is heated, under the influence of which it disintegrates, the pressure on the nerve roots decreases, and the pain syndrome disappears.
The operation is carried out no more than an hour, a few hours after it, the patient is allowed to go home, full rehabilitation lasts 1.5 months.
Laminectomy
The operation of the case under general anesthesia - the surgeon makes an incision up to 10 cm, through which part of the vertebra is removed, to which the nerve process is pressed by the hernia. After the operation, rehabilitation takes place in a hospital for several days, the pain syndrome recedes immediately. Among the risks, the danger of infection and damage to nerve endings are distinguished.
After the operation, the rehabilitation period is important, but this is not the time to lie on the couch. During this period, physical therapy is needed, it will help strengthen the muscle frame and reduce the risk of relapse.

“Herniated disc” - such a diagnosis is becoming more common and the reason for this is a sedentary way of life, but the treatment of this ailment stimulates controversy and discussion.
What is a herniated disc?
Herniated discs can occur after injury or the spine. It can cause compression of nerve structures.
The vertebrae are interconnected by intervertebral discs in the spine. They have a high density and consist of an elastic core located in the center of the disc, the core is surrounded by strong rings of connective tissue. Numerous diseases of the spine are directly related to the destruction of the intervertebral discs.
Today, only a few indicators affect the purpose of an operational decision:
- does not go away within 6-7 months, is not removed by anything other than narcotic analgesics;
- progressive muscle atrophy of the limb, paralysis of the limb that does not go away;
- the functions of the pelvic organs are impaired;
- progressive spondylolisthesis.
Not specified manifestations of such a hernia require only a conservative solution. With hernias, acute and prolonged pain can occur, which often prevents patients from objectively judging their condition.
With constant aching or "shooting" pain in the back, lower back, neck, which do not go away for a long time, you should pay serious attention to your health. Perhaps such pains indicate the presence of a herniated disc. This is an unpleasant dangerous disease that requires surgical treatment, otherwise the disease can progress and cause serious damage to the health and well-being of a person. Herniated disc occurs when the nucleus pulposus of the intervertebral disc is displaced with rupture of the annulus fibrosus.
Where does a vertebral hernia occur?
Intervertebral hernia can be localized in different parts of the spine. The most common hernia is in the lumbosacral spine. In this case, the pain can be given to the back, lower back, hips, legs, feet, buttocks. Disorders of the intestines may occur, Bladder, men may have problems with potency.
Less common is an intervertebral hernia in the cervical spine. Headaches may appear, there may be pain in the arms and shoulders, frequent dizziness appears, memory functions are impaired. When between vertebral hernia thoracic region pain is also in the thoracic region, in the interscapular region, scoliosis may appear.
An intervertebral hernia appears, as a rule, from an uncomfortable workplace and wrong position during the performance of professional duties of drivers, surgeons, welders, etc. Often intervertebral disc defects arise from regular heavy lifting. The dangers of intervertebral hernia are also exposed to those who receive a spinal injury due to an unsuccessful fall, various fractures.
Treatment methods based on the size of the vertebral hernia
Hernia treatment should be started as soon as it is found. The more run intervertebral hernia, the more time and effort it will take to relieve pain. If an intervertebral hernia is suspected, the doctor will order CT or MRI. Basically, experts recommend using magnetic resonance imaging as a method for diagnosing an intervertebral hernia - it is the safest for health and provides the most accurate data on the location of the hernia and its size.

An intervertebral hernia is treated in various ways: conservative and surgical. The method of treatment is determined by the size of the spinal hernia. If the displacement has just begun to occur, and the size of the spinal hernia is about 2 mm, medication, manual therapy, spinal traction, etc. can be dispensed with. A medium-sized protrusion, for example, a 5 mm disc herniation, can also be treated with a non-surgical method. With a large size of a hernia of the spine of 8 mm, treatment is prescribed, including surgical. However, surgical intervention in this case is not the final stage in the treatment of a hernia of the spine. After the operation, the patient is prescribed medication, massage, physiotherapy procedures, and sanatorium treatment is recommended.
Let's talk in more detail about the treatment of a hernia, based on the size of the displacement. The dimensions of the intervertebral hernia of the lumbar and thoracic spine are subdivided as follows: a small protrusion from 1 to 5 mm. Medium protrusion is considered to be from 6 mm of protrusion of the intervertebral disc, and large - more than 9 mm. Sizes of a hernia of the cervical spine: small - 1-2 mm, large protrusion - 5-6 mm. Thus, the need for surgical intervention is most often determined based on the size of the vertebral hernia.
The dimensions of the intervertebral hernia of the lumbar spine
Intervertebral hernia lumbar 3 mm requires outpatient treatment, home treatment, which implies traction of the spine, therapeutic exercises.
A spinal hernia of the lumbar spine of 6 mm is considered average, therefore, it implies more serious outpatient treatment with the use of additional methods. Manual therapy, physiotherapy treatment (massage, ultrasound, spinal traction), physiotherapy exercises. However, when asked whether surgery is necessary to treat a 6-7 mm lumbar disc herniation, doctors answer that no surgical intervention is required.

But with an intervertebral hernia of the lumbar spine measuring 12 mm, surgical intervention is required if symptoms of spinal cord compression appear and when elements of the “horse's tail” appear.
Sizes of a hernia of the cervical spine
An intervertebral hernia up to 2 mm in the cervical spine is considered small; manual, medication, physiotherapy methods are provided for its treatment. A hernia of the cervical spine measuring 3 mm, like an intervertebral hernia of 4 mm, requires urgent outpatient treatment in order to avoid further trauma to the site. An intervertebral hernia in this area of 5-6 mm still allows for outpatient treatment. But if an intervertebral hernia of the cervical spine larger than 6 mm is detected, it requires urgent surgical intervention.
Regardless of what size and in what section the disc herniation is found, the sooner treatment begins, the better. If a hernia of the spine is detected in time, there is every chance to get rid of the disease or at least relieve symptoms, ensuring the proper level of quality of life. In addition to outpatient treatment, it is effective to use. But only as a supplement, without replacing them with conservative treatment (medication, manual and physical therapy).
| The dimensions of the intervertebral hernia | ||
|
Lumbar and thoracic spine |
||
| The size of the intervertebral hernia | Characteristic | Treatment |
| 1-5mm | Small protrusion size | Outpatient treatment needed, probably home treatment- spinal traction, remedial gymnastics |
| 6-8mm | Average size of a vertebral hernia | Outpatient treatment required, no surgery needed |
| 9-12mm | Large protrusion size | An early outpatient treatment is necessary, surgical intervention is indicated for symptoms of compression of the spinal cord and elements of the "cauda equina" |
| More than 12 mm | Large prolapse or sequestered hernia | Outpatient treatment is possible. But when symptoms of spinal cord compression appear, the patient must undergo surgery. |
|
Cervical spine |
||
| The size of the intervertebral hernia | Characteristic | Treatment |
| 1-2mm | Small size of herniated disc | Urgent outpatient treatment |
| 3-4mm | Average protrusion size | Urgent outpatient treatment needed |
| 5-6mm | Large size of the vertebral hernia | Outpatient treatment possible |
| 6-7mm and more | Large size of intervertebral hernia | Surgical treatment needed |
A hernia of the spine can form in any of its parts. Most often, the lower back is affected (up to 90% of all cases), then the neck. In the thoracic region, a hernia forms less often. The lower back is more exposed to physical stress than all other parts of the back. Under their action, the deformation of the intervertebral discs occurs. Their protrusion beyond their natural boundaries is called protrusion, and is considered normal if it passes with the disappearance of the load. When the changes persist and develop, we can talk about pathology. Treatment of a hernia of the spine directly depends on its size and the severity of the course of the disease.
Dimensions (edit)
With constant or excessive loads, with age, dystrophic processes occur in the intervertebral disc. The fluid content in it decreases, the fibrous ring loses its strength and elasticity. The constant and uneven pressure of the nucleus pulposus on it causes the appearance of microcracks and, over time, if not treated, inevitably leads to rupture. Such a pathological process can be divided into several stages:
- Initial degenerative changes in the intervertebral disc.
- Protrusion (bulging).
- Hernia (prolapse or drooping).
- Sequestration (separation of a fragment of the nucleus pulposus).
A hernia can protrude outward (the safest option), into the spinal canal or sideways (both conditions are dangerous). The severity of the disease is determined not only by the direction of the protrusion, but also by its magnitude. For each part of the spine, the size of the pathology that appears has its own meaning. If for the lumbar spine, a protrusion of 1–3 mm would be considered more of a protrusion, then for the cervical spine it is already a full-fledged intervertebral hernia, and quite large and dangerous.
- 1 to 5 mm - slight protrusion. In the cervical spine up to 2 mm, in the thoracic and lumbosacral up to 5.
- 6 to 8 mm - medium protrusion. If the localization is in the cervical spine, then its 5-6 mm can be considered large, and 2-4 mm average. For thoracic and lumbar, the maximum indicator is 8 mm.
- From 9 to 12 mm - large intervertebral hernia. Protrusions of this size are characteristic of the thoracic or lumbar regions.
- From 12 mm or more - large prolapse or sequestration.
The size of the hernia does not always matter. The direction of protrusion is much more important. If the hernia protrudes into the spinal canal, then even the smallest danger (1-3 mm) is present. Spinal cord compression can cause severe pain and paralysis.
An intervertebral hernia can be treated in different ways - conservatively or promptly, it all depends on the size.
Pathology of the cervical spine is considered the most difficult to treat because of the small size of this part of the spine, the small size of both the vertebrae and the discs separating them. But most often, patients complain not to the neck, but to the lumbosacral region. Formations up to 15 mm are found here.
Conservative treatment

Lumbar and cervical hernias are considered the most dangerous. In the neck, they can cause paresis. upper limbs and cerebral ischemia, in the lower back interfere with the full functioning of the musculoskeletal system and affect the work of internal organs.
An operation can be dispensed with for a hernia in the lower back up to 8 mm, in the neck - up to 2–4 mm. Treatment in this case is symptomatic (relieving pain, eliminating tension) and improving the flexibility of the spinal column:
- Medication.
- Manual therapy.
- Physiotherapy.
The main thing with conservative treatment intervertebral hernia - do not miss the moment when it can still be effective.
Medications
Basic drug therapy includes several areas: elimination of the causes, removal of symptoms, blocking the pain syndrome if necessary. The main groups of drugs for the treatment of intervertebral hernia:
- Non-steroidal anti-inflammatory drugs (NSAIDs). Diclofenac or Movalis (NSAIDs) are often used. The drugs block the production of cyclooxygenase, which is involved in inflammatory process, reduce fever and relieve pain well.
- Chondroprotectors and preparations based on hyaluronic acid. Usually Teraflex or Alflutop (chondroprotectors) is prescribed. They are well tolerated by patients, nourish the cartilaginous tissue of the intervertebral disc and strengthen its structure, thereby preventing the destructive process and inhibiting the progression of the disease. Karipain Plus or Rumalon are preparations containing hyaluronic acid. They help to increase the fluid level in the nucleus pulposus and increase the elasticity of the annulus fibrosus.
- Muscle relaxants. Mydocalm relaxes stiff muscles. It is used only as directed by a doctor.
- Improving blood circulation. Trental or Pentoxifylline strengthens the walls of blood vessels, relaxes smooth muscles and, with complex therapy with Milgamma (B vitamins) and Actovegin (neuroprotector), reduce the lack of oxygen.
- Means for the protection of the gastrointestinal tract. Gastal or Almagel prevent damage to the gastrointestinal tract when using NSAIDs. They are prescribed in combination with non-steroidal drugs.
- Antidepressants. Sertraline or Insidon allow the body to fully recover during sleep.
Blockade

Spasm and pain are relieved with an injection of anesthetics and corticosteroids. This procedure can take up to several weeks. The duration depends on the route of administration of the drugs and the response of the body. The blockade with a hernia of the lumbar spine is divided into two types:
- Local - periarticular, intraarticular or epidural.
- Segmental - paravertebral.
Only a qualified specialist with experience in such treatment can determine the need to prescribe a blockade and decide in what way it will be carried out. The doctor must find out if the patient has contraindications, and take into account all the risks in case of possible complications.
The use of a blockade for intervertebral hernia of different sizes has several advantages:
- Fast results. The anesthetic is delivered directly to the lesion.
- The minimum effect of the administered drugs on the entire body due to local application.
- Repeated use of the procedure provides a stable, long-term relief of pain syndrome and rapid elimination of the inflammatory process.
Physiotherapy
It can be performed only after consulting a doctor. The nature and burden of exercise should be consistent with previous therapy (eg, surgery), if any, or meet specific objectives, if used as a treatment.
Unlike exercises for the cervical spine, which are performed while sitting, gymnastics for the lumbar region should be done in a prone position. For the upper part of the spine, the exercises are relaxing, and for the lower part, complexes that strengthen the muscles of the lower back are necessarily connected.
Allowable exercise therapy complex for lumbar hernia:
- Lying on your back, straighten your legs together, stretch your arms along the body.
- Tighten and relax your abdominal muscles.
- Raise the pelvis slightly and stay in this position for 10 seconds.
- Lie on your back, alternately pulling your legs bent at the knees, try to press them to your chest.
Physiotherapy exercises are prescribed for hernias in the lumbar spine, no more than 6 mm in size. In other cases, it is used as a restorative procedure after surgery.
Manual therapy

In addition to the main treatment, intervertebral hernia of the lumbar (thoracic, cervical) spine, there are auxiliary measures to enhance its effect, consolidate and prevent recurrence of the disease.
Massage for intervertebral hernia is prescribed exclusively during the period of remission. The main goal is to reduce muscle tone, improve blood flow, relieve pain, and speed up rehabilitation. The manipulations of the masseur should be gentle and careful. When kneading, the patient should not feel pain.
Physiotherapy
Treatment with weak currents has been successfully used for a long time. This is, for example, its diadynamic variety or electrophoresis. Electrodes attached to the patient's skin under low voltage have either a local irritating effect, or help the drug to penetrate to the lesion.
Electrophoresis procedures with Novocaine or Lidocaine in the treatment of intervertebral hernia can significantly reduce the amount of non-steroidal drugs used, thereby reducing the negative effect of the latter on the body.
Operative treatment
Surgical intervention in the treatment of a hernia of the lumbar spine is considered a measure of extreme necessity when the size of the protrusion is 12-15 mm. It is advisable to use this method only in the case of a long and fruitless struggle, a strong influence on the internal organs from the very beginning of the development of pathology or during a critical exacerbation.
Microdiscectomy
The operation is performed under high magnification or a microscope. A neurosurgeon with a minimal incision (up to 2 cm) and an almost jewelry instrument removes any type of intervertebral hernia. Damage from the doctor's manipulations is insignificant (the yellow ligament is partially removed and, in rare cases, the vertebral arches are excised), so relapses are minimized.
An indication for microdiscectomy is usually considered:
- Pain that does not go away even when using the blockade.
- Compression of the spinal canal.
- Hernia up to 5–6 mm in size.
The recovery period takes little time, since muscles and ligaments are not affected during the operation. The patient can sit right away, the pain syndrome is insignificant.
Endoscopic microdiscectomy

State of the art operation. A micro-incision is made (no more than 0.5 cm), into which the endoscope is inserted. With its help, the hernia is examined, and then it is removed. The surgeon sees all manipulations on the monitor.
The main advantage of this technique is the absence of a rehabilitation period. The patient is on his feet immediately after the procedure. The weak side is the limitation of its use depending on the size of the protrusion. The possibility of carrying out this minimally invasive operation is determined by the size of the hernia up to 6 mm.
Laser nucleoplasty
Removal of an intervertebral hernia with a laser can be either an independent treatment or be used in combination with a conventional operation (at the final stage of endoscopic microdiscectomy). The light guide inserted through the puncture hole heats the protrusion. The vaporized liquid is removed through a needle.
The method allows you to remove the hernia without causing any harm to the patient. Laser nucleoplasty is a minimally invasive procedure with a minimum possible complications, however, the patient will have to spend at least 3 days in the hospital. The operation is effective in young patients with a hernia size of no more than 6 mm.
Even the most modern method of treatment requires a responsible attitude to recovery period after operation. Follow the recommendations of the attending physician, lead a healthy lifestyle, do not avoid feasible physical exertion and undergo regular examinations to prevent the formation of new intervertebral hernias.
